How Sonder’s medical team supports a workforce in distress [Video]
Insights.
The pandemic has exacerbated customer aggression and workplace distress, as well as highlighted gaps in employee support. What more can be done? How does Sonder’s medical team help our customers and their team members?
At our recent event for retail and hospitality leaders, our medical experts Dr Jamie Phillips, Louise Butler and Kimi Powell shared their stories and experiences.
Presentation
Presenters
Panellist 1:
Dr Jamie Phillips MB ChB, AFCHSM, DIMC, RCS(Edin), MRCGP(UK), FACRRM(EM)
Dr Jamie Phillips is a Commando-trained Military Officer, who served for 20 years in the UK Armed Forces and Australian Defence Force as an embedded doctor and operational Commander on multiple combat operations around the globe. He is a specialist rural and remote physician, with advanced specialist training in emergency medicine.
As Medical Director and Head of Member Support at Sonder, Jamie shapes the health culture within the organisation. Fulfilling both leadership and clinical roles, he is responsible for the quality, safety and responsiveness of the support provided. A practising physician, Jamie maintains his currency working in emergency medicine and as a lecturer at Bond University.
Panellist 2:
Louise Butler
Louise Butler is an endorsed clinical psychologist and authorised supervisor who has spent her career treating and supporting people experiencing a mental health crisis. Louise is the Head of Psychology at Sonder.
In her former position as the clinical psychologist in a secure adolescent mental unit in a children’s hospital in Sydney, Louise delivered advanced mental health care and support to children and adolescents, and their families, who were experiencing significant and complex mental health issues.
Prior to this, Louise worked with the Department of Communities and Justice, providing life story and mental health care to young people in out-of-home care.
Panellist 3:
Kimi Powell
After spending many years in emergency care, Kimi now manages Sonder’s 24/7 team of nurses. She brings a unique approach to holistic care, influenced by the Mãori health model “te whare tapa whã”.
Transcript
Craig Cowdrey (Sonder CEO):
So, our next session, as I flagged, is going to be hearing from some of our staff here at Sonder and the cases that they have been dealing with that are related to this customer aggression/customer hostility. Hearing about how we tackle it here at Sonder, providing some advice and some practical tips on how you and your people can help to tackle these as well.
So, I’ll invite the guests to come up and take a seat, and I’ll do a quick introduction as well. So, I’ll invite Louise Butler, our Head of Psychology to come up please, Kim Powell, our Director of Nursing, and Dr Jamie Phillips, our Medical Director. Please have a seat.
So, at Sonder, we apply the Sonder Holistic Wellbeing Model, and the architects in particular are sitting here in front of you – Jamie and Kim. Now, I’m too proud to not mention this, but the Sonder Holistic Wellbeing Model is what allowed Sonder to win Australia’s Most Innovative Company Award last year out of 700 technology companies across the country. And it’s this approach that we take to really be broad in how we understand a person’s issues, and cutting across medical, personal safety, and mental health as well, to really address what might manifest as a symptom for an employee – anxiety, stress, depression – but also to dig in under the hood and understand what is causing that in order to tackle that as well. And we see that about 55% of cases that we deal with cut across these different pillars, so it’s important that we take that broad approach. It’s also what allows us to have up to ten times more engagement with an employee base, compared to, for example, an EAP provider.
But it’s that model that you’ll be hearing a bit more about now, and also the cases that have come through that model and what that means for your organisations and how you can better help your people.
So, I’ll hand over to the team for the next 15 minutes or so.
Dr Jamie Phillips:
That’s great, thanks Craig. What the hell do a doctor, a psychologist and a nurse know about customer hostility? Sadly, it’s a big part of our daily lives as clinicians and as medical support staff. Every single day in healthcare, we experience aggression, hostility, and violence, particularly in mental health and particularly in emergency medicine, which is mine and Kim’s background.
In a New South Wales study actually – I was reading it last week – in 2018, they surveyed ED staff in New South Wales, and they found that 100% of the respondents to the study reported violence and aggression in the workplace on a weekly basis. So, it is a problem. And certainly, the clinicians and the safety specialists you see there and up at the top there all have a deep, lived experience of aggression, hostility, physical violence and sexual violence in the workplace. I mean, I was at work last night in ED as the boss, and I sadly witnessed overt aggression and hostility towards my staff, which as a clinician breaks my heart, but as a leader, breaks my heart. How do I protect my people? How do I protect myself? How do I protect my patients who are there using the service as well – my customers – and still maintain a therapeutic relationship? Because they’re there, they’re in need, they need something from us, but they’re reacting aggressively. And the natural reaction is either defence – flight, or aggression – fight. Neither of that is going to help the patient. And neither of that is going to help me. And it’s something certainly we deal with – don’t we, Lou – every single day.
Louise Butler:
Yeah, absolutely. Do you think it’s timely for me to introduce a case that kind of represents how we deal with…
Dr Jamie Phillips:
Yeah, I think that’s a good idea. Do that, and then we can maybe unpack it.
Louise Butler:
Sure, okay. So, obviously we get cases all the time, and in my past history working in child protection and in the hospital system, and now here at Sonder, I’m very used to working with distressed members. I just want to flag here too, I don’t use the word aggression. As a clinical psychologist, I use the word distressed.
So, in my job, I’m used to seeing people on the worst day of their lives. They’re seeing me because they’re really overwhelmed; something horrible has happened. it could be trauma, it could be their own mental health, it could be a combination – a medical mental health issue, a safety concern. You know, people have very different backgrounds and life stories, cultural backgrounds, that sort of thing.
So, since I started joining Sonder, which was August last year, I’ve been working with people to say, can we view this in a different light? So as Jamie said, if we’re going to be defensive or get upset and angry ourselves, you can’t help the person in front of you. So we have to calm the situation down. I take on a curious stance with people. So, if they’re looking really agitated and distressed, it means, okay, I should be able to help somehow here. Even if it’s just to help them calm down, understand their position, and see if I can help personally, or can I refer them to someone who can? So you give them the space to tell their story, so why they’re so upset and angry at this point in time, and what can I do to help? Then you’re on the same page with them and they can see you’re an advocate. That means you’re on the same playing field, and that gives you both space to work with each other.
So that’s my sense on when you’re dealing with someone that looks to be aggressive or upset – it usually means they’re having the worst day of their lives. So this change in perception kind of, I think, takes the agitation out of it for both of you.
So there’s that part of it. So, I’ve introduced that to the mental health pathway system in Sonder. So if we go through a case, Kim, a typical case, that’s de-identified.
Let’s think about a lady in her early 20s, she works in a workplace that’s quite busy, a shopfront, through the COVID era. She’s minding her own business, doing her job, and there’s a customer there that looks pretty upset and distressed; they’re throwing items off the shelf. It’s getting close to other customers. She steps in and says, “Can I help you here? I can see that you’re upset”.
She gets something pegged at her face, so she’s hit and bruised as well. Then a manager gets called to try and assist, and then the situation gets worse.
So in this situation, the member has gone back to the manager when things calm down, and the manager said, “Look, I can see you’re upset by the situation – understandable – take a break and then come back when you’re ready”.
So that’s what’s happened.
Then time passed, and the member wasn’t coping well. So apart from the physical injury, she also had mental health symptoms coming up for her. She didn’t tell the manager that because she wasn’t sure how to address that with the manager. So then in about a week’s time, she called Sonder, and she came through our support centre.
Do you want to talk about the nursing pathway?
Kimi Powell:
Yeah, sure thing, thanks, Lou. What we do here as nurses, when they present to the call or chat, to the support centre here, we do a bit of triage, see where it needs to go. We try and address the most immediate thing for treatment at that time, so physically assaulted, we need to address those. We always have to medically clear – and it’s the same when you go into a hospital – we have to medically clear people before we move on and see what further supports they need.
So we address the injuries. “How are you going?” “Yes, I do have headaches, they’ve been ongoing.” We dug a little deeper into that – she’d been to the GP, sorted all that out – I think she had a scan, I’m not quite sure. But that came back NAD, that came back good, everything was fine there.
Louise Butler:
No nurse talk, here.
Kimi Powell:
No nurse talk, sorry about that.
So, then what we did was, the other issue that she had that was affecting her sleep, her activities of daily living and for her to be able to function productively at work and things. She’d had a few days off and stuff like that. So, yeah, she did need further support. We use a really good wellbeing model for assessment – it’s holistic -and we ascertained, yes she does need further support. She also had a history, didn’t she?
Louise Butler:
She did. So, the way our support centre works, they come in, the situation is unpacked to a certain point, so they know, is it medical, mental health, safety, wellbeing? And then the priority situation is dealt with first. So, in this case, it was medical, because she was hit in the face and had bruising, and she had seen the doctor and had headaches.
But through that unpacking, when it went to a nurse, they are trained here to also unpack mental health issues. And then she started to allude to things like having a trauma background and having a previous incident in the same store. So it was quite evident that there were growing mental health concerns as well, and she was struggling to return to the workplace because of flashbacks and things like that.
So through our service here, that gets referred to the psychology team, and we’ve got an internal team called the CAT team – the Crisis Aversion Team. So when we have cases like this when we feel like they’re struggling to go back to the workplace, so it’s workplace-related, there are mental health issues, there’s been a medical issue as well and potentially workplace, like WorkCover situation, we deal with that case and we review it, and we work out the best mental health pathway. So we have a few options within Sonder.
So it was allocated to one of the psychologists in our psychology team, and they unpacked the case with the member, did an initial assessment, and uncovered that there was long-term anxiety for this person and low-level depression. She used to cope by abusing alcohol. She had overcome her alcohol abuse about a year before this incident, but after this incident, she started drinking again to cope. There was also a sexual assault within the same workplace about six months earlier. So combined, there were a lot of issues with her mental health.
So she was allocated to a psychologist in our team, and that included, with her consent, speaking to the manager, to work out a return to work plan.
So, I think that’s the summary of the case.
Kimi Powell:
Yeah. The trends that we’re seeing and the calls that come through to us all sort of resonate the same. People are feeling isolated, and they’re feeling like – I’m trying to be delicate here – the management structure probably isn’t as supportive or advocates on behalf of them. Because as we heard earlier, do you take the side of the customer or do you take the side of the staff member?

So, we’re seeing that and we find that what people are actually wanting – and we come from a place of unknowing to a place of knowing, so we try and get alongside – and it’s a journey for us, and it’s journey for them. We flatten the power gradient, but us being clinicians, it’s not about us being clinicians, it’s about us listening to their stories and what matters to them. Because if it matters to them, it matters to us.
Jamie taught me that when I came here. He said, “Look, it doesn’t matter what it is, if it matters to them, it matters to us”.
So, we try and go on a journey with them – what do you need – and we just listen to them. And a lot of people, that’s all they really want, they just want to be listened to and they want to be heard. They don’t want to be told, you need this, this, this, this this – that’s what they do in ED – you’ve got 30 seconds to tell me why you’re here in the middle of the night – go! And that’s what we do – we used to do that. I used to do that. Jamie did that.
Louise Butler:
I never did that.
Dr Jamie Phillips:
So, the golden child sits in the middle.
Kimi Powell:
I always joke about this with Lou. I always say the only difference between a psychologist and a patient is a set of keys. All the time in the world to talk to people. We don’t – we like fast, fast, fast.
But here, we take that time to hear, and that’s what’s meant the most to me. And Jamie and I, when we came here, it was like, how can we make healthcare different, how can we make it meaningful for partners and for members? You know, we want to be able to provide value, meaningful value, for partners and members that come through.
But here, we take that time to hear, and that’s what’s meant the most to me. And Jamie and I, when we came here, it was like, how can we make healthcare different, how can we make it meaningful for partners and for members? You know, we want to be able to provide value, meaningful value, for partners and members that come through.
Louise Butler:
I know we’ve got quite a short speaking slot here, so one of the take-home messages from this case too – there’s a theme that I see as Head of Psychology – managers really want to help their staff. COVID has really brought that out. So, the one positive from COVID is, mental health is now top priority for everybody. You’ve either seen someone that’s really suffering or you’re suffering yourself. And it’s not just a one-off, it’s repeated. You’re in lockdown, you’re out of lockdown. You change your hours at work, you’ve increased your hours at work, then you had to take a break. So, there’s a lot of people in trauma, and pre-COVID, people on their worst day went to emergency or to a psychologist. Now everyone’s having their worst day repeatedly. So this is unfolding in the public. So how do we all deal with this when we’re all feeling fragile and our resilience is low?
And I find the theme here at Sonder – managers want to do their best, they want to help their staff, but they don’t know what to do because they’re also poor on resilience. They don’t know how to speak about mental health. So, Sonder is spending a lot of time providing educational support to the managers. So this distress is quite contagious. And I say, don’t be scared about it, own it and know that you’re in it, and you’re helping as many people as you can. Because then it’s the fear that creates more distress.
So in this particular case, you’ve got the initial customer. We don’t know his life story because he’s not a member here, but we would have unpacked that if he was. Then we’ve got the staff member, who is also distressed from the incident, plus her own life story. Then we’ve got the manager who is distressed because they don’t know how to help this member. And then you’ve got privacy issues on top of that, so you don’t know how to ask about mental health history. And then you’ve got the workplace, while these people are taking time off to work out how to help themselves.
So you can see it’s like a contagion effect, and it’s global, and it impacts on everyone at the workplace and at home. But I just don’t want people to be scared about that. We’re all in the same boat, so just be curious and help each other.
Dr Jamie Phillips:
And I think that’s the key thing. I talked about this a few months ago, didn’t I, at a conference. Nobody ever asked managers to be mental health experts. None of you were ever asked to do that. You naturally assumed that role because you cared. But then you reach a point where you start to get unsafe, you feel concerned. And we hear a lot of leaders coming through saying, “I don’t know what to do here,” and we say, “Brilliant”. That’s the start point we want.
Louise Butler:
Absolutely.
Dr Jamie Phillips:
Help me, help them, help us. And it’s very powerful for us. We don’t see aggression or hostility as that, we see it as distress. And rather than having a hostile face-to-face, just thinking of it as distress. If you saw somebody on the street who was distressed, you’d stop and help, wouldn’t you?
Louise Butler:
Well, maybe not. Not everyone does do that.
Dr Jamie Phillips:
Not everyone does.
Louise Butler:
Some people are too scared.
Dr Jamie Phillips:
Maybe some people are too scared. But if you saw someone who’s distressed, rather than somebody who was aggressive, you’d want to stand alongside them and say, “How can I help?” It’s no different with customer aggression. If you do nothing and you take nothing away from this, I’d say these three things.
Number one, reframe customer hostility as aggression yourself and within your team as distress. That customer is distressed. And as soon as that button flicks in your mind, you think, how can I help here. And it takes the heat out of the situation. It’s what we did last night in ED. Clearly, you are distressed, not, “We’re getting security”. How can I help you? I want to sit down alongside you. The heat’s gone. It’s protective for me, and it’s protective for the customer, and it’s protective for everybody else around.
Second thing is, nobody ever asked you to be a mental health expert. If you don’t know what to do, just say, “Hey, we need help”.
Louise Butler:
And at that point, make sure you know who your EAP service provider is, because it’s really key in this era. Because, you know, people tended to ignore that fact prior to COVID, but now it’s really important. And actually trust the EAP service. I mean obviously I work for Sonder, so I’m going to say we do it brilliantly. But that’s the key. So if you’re a staff member, if you’re a manager, if you’re a higher exec, speak to your EAP service if you’re struggling. The sooner you get help, the easier it is to manage and to recover, and there’s less distress for people around you.
Dr Jamie Phillips:
And the final thing is complexity. These situations are not just safety, not just mental health, not just medical assault. More often than not, and that’s what our data shows, it’s all three. And if you just try and solve this situation with just a mental health silver bullet, the other two problems are going to be there, and you’re never going to fix them. And that’s what causes the real problems. So open your minds, think about it a bit differently, and ask for help.
Kimi Powell:
Always remember too that nobody gets up in the morning and goes, I’m going to go out for lunch and I’m going to spit in the face of the waitress. Nobody gets up and does that and thinks, I’m going to go and punch John down the road for not giving me the right coffee. There’s always a set of events that happens before then, and you just happen to be that one person almost in the wrong place at the wrong time.
Dr Jamie Phillips:
That’s great. I think we’re at time are we Jason?
Kimi Powell:
Jason’s pacing.
Jason Kerr (Sonder colleague):
We’ve actually got a couple of extra minutes. Thank you all for that session, I’m sure everyone found it very interesting and informative. We do have a couple of extra minutes if there are any questions from the audience, if you’d like to take the opportunity.
Craig Cowdrey:
Sorry, we’ll just get the microphone to you so the online group can hear.
Nancy Mendes (PwC Australia):
Hi, I’m Nancy Mendes from PWC. A great panel discussion, thank you very much for that insight. Sonder is known for mental health support, but I did hear that you’re doing holistic assessment when a distressed call comes. What do you do with that extra bit that you find out about the person who’s distressed that’s not mental health related? You know, how do you offload that and ensure that the person is cared for holistically?
Kimi Powell:
In terms of medically, are you talking about, or through the course of the assessment?
Nancy Mendes:
Through the course of the assessment.
Kimi Powell:
What we do is try and address the most important thing at that time that they will need. They may need this other myriad of things going on behind the scenes for them, but it’s pretty much the one thing that we can get them that will be the most value for them, the most help for them at that time. Don’t we, Jamie?
Dr Jamie Phillips:
Yeah. I think that’s what we do, we apply a holistic model that doesn’t look at things through a myopic view, does it? Every single case gets considered through medical, mental health, social and family. And by family, we don’t mean your direct family, we mean your work family as well. The people in your community. And in spiritual. And actually, we don’t mean in a traditional spiritual sense, we mean what does this mean to me right now and where am I going and what does this mean for me moving forwards? Every single time someone reaches out to us, we explore all four options.
Kimi Powell:
And we consider all their cultural aspects as well. I’m not talking about I’m from New Zealand and somebody’s from Australia; it’s all about how they see themselves in the world, where they fit, their thoughts, their beliefs, their feelings. So we address those. It’s not a tick box that we go through, but through a conversation. And we find out what means the most to you and things like that. So we sort of work through that as well.
Dr Jamie Phillips:
And through that, you build trust. We’re in the trust business. If you actually truly hear, listen to, and validate it, you get trust. And something Kim and I are very passionate about is follow-up. If people are happy to have it, we follow up 100% of our people, because follow-up builds trust. We’ll reach out and say, “Hey Kim, I know you had the worst day of your life yesterday, we just want to know how you’re getting on”.
And that’s when they say, “Oh, now I’m doing fine,” because we’re all conditioned to do that. We’ll say, “Really, you mentioned a couple of other things. Is there something else we could do for you right here?”
And that’s the next step up to build more trust. And then we follow that up again. We build a bit more trust. And we’ve got our own team of doctors, nurses, social workers, midwives, psychologists, and they’re people we trust. And we can give a warm handover and serve some trust. So I will say, “Hey, I’m going to refer you to Lou, she’s a good friend of mine, I work with her”. Lou’s got a warm handover, she says, “Jamie’s told me all about you”. There’s that surging of trust with patients, and they don’t have to tell the story again.
Does that answer the question?
(Claudine Mardini takes the microphone.)
Dr Jamie Phillips:
I’m scared, Claudine.
Claudine Mardini (Woolworths Group):
You should be.
(Claudine smiles.)
I’m Claudine from Woolies. I’ve just got a question. You speak a lot about leaders and not being trained or have limited training with mental health and distress situations. What would your recommendations be for people like us in the workplace that are safety and health and wellbeing would be best for our team? Would it be mental health first aid so we can help our leaders? Are there other things that we could do to help our team and our leaders to be better in this area?

Dr Jamie Phillips:
Should I start and then hand to you?
Louise Butler:
Sure.
Dr Jamie Phillips:
Yeah, so I think at a sort of leadership point of view, just be inquisitive, Claudine. I know you well because we have conversations every week, don’t we? But be inquisitive, and don’t be afraid to care, and as Lou said, accept that you’re in it. Enjoy the chaos, embrace the chaos, because that’s really where the magic happens. The moment you try and parcel it off and put it up to something simple, you’re not leading. And I speak as somebody who has led for many years, but you don’t need to be a clinician. Psychological first aid is fantastic. It gives you a framework and a shared mental modelacross the team that it’s okay to care. You don’t need to be a specialist clinician. But it also teaches you to escalate, doesn’t it? Appropriately.
Louise Butler:
Absolutely. Yeah, that’s what psychological first aid is, if you’re not familiar with it. So it is for people exactly in that position, where they are working with people where it’s helpful to identify early on if there’s someone that’s suffering with mental health issues. And how to have that conversation, for instance, “Are you okay? Well, are you really okay?” And recognise when the conversation gets to a point, and you realise, I need specialist help, okay, well who is our EAP provider, or who are we partnered with? How can I get them support? And it could be helping them call their own emergency contact and taking them to the GP. Or it could be giving them a room to phone the EAP service.
Dr Jamie Phillips:
But that’s the big problem, Claudine, as you know, it’s access block. In healthcare. Mean wait time I think for mental health at the moment in New South Wales is 18 weeks is it, in the community? Or is that generous?
Louise Butler:
No, that’s generous, yeah.
Dr Jamie Phillips:
Okay, maybe more than 18 weeks. And that’s what we’re trying to solve. ED last night, seven and a half hour wait to be seen. That’s in a capital city in one of the richest countries in the world. It’s not good enough. And that’s what we want to do with our leaders, is when they come to us and they say, “I have a problem, I don’t know how to fix it, I’ve been through my steps, can you connect me with what I need?” 100% – leave it with us. And then we reach out, as you know Claudine, to the leader. We’ll say, “You’ve been through a lot”. Because we’ve got the individual who’s dealing with the problem, but then we’ve got the leader as well, and we often end up supporting both, don’t we?
Louise Butler:
Well, we do. So that’s why each case takes a fair bit of time, but that’s what we’re here for. Because it impacts on everyone. So you have a distressed member who has their own life story, you have the manager who doesn’t know how to help that person in the workplace or how to get them back to the workplace, and then you’ve got upper management.
But one thing I want to add is, if upper management can talk about mental health – not necessarily their own, because everyone has privacy – then it becomes a topic that can be talked about at work and people feel supported from the top down. So you’re not going to get people in the workforce on the floor talking about mental health if their own managers don’t talk about it or the execs don’t talk about it. So it’s got to be an approved topic that is part of the normal discourse in a company.
Dr Jamie Phillips:
And so, a poster in the tea room, doesn’t cut it. That’s not leadership. What that is, is dispensing your moral obligation to care about your people. It’s not true leadership. True leadership is being vulnerable.
Want to learn more?
Read the full event recap of our event, The real impact of customer hostility.
For more information about how Sonder can help you rethink your student and employee support, we invite you to contact us here.
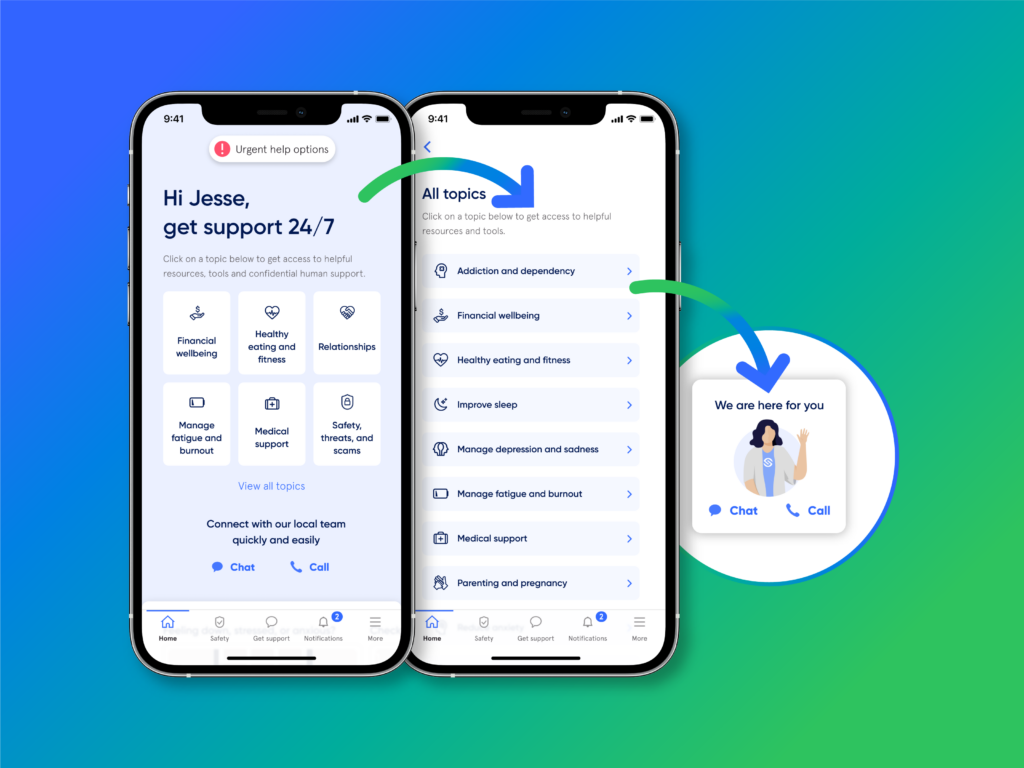
About Sonder
Sonder is an Active Care technology company that helps organisations improve the wellbeing of their people so they perform at their best. Our mobile app provides immediate, 24/7 support from a team of safety, medical, and mental health professionals - plus onsite help for time-sensitive scenarios. Accredited by the Australian Council on Healthcare Standards (ACHS), our platform gives leaders the insights they need to act on tomorrow's wellbeing challenges today.
Related posts
There's so much more to share
Sonder is reimagining health, safety and wellbeing support. Sonder proves human centric care leads to earlier intervention. Sonder impacts one person at a time to drive meaningful change across an organisation. Sonder understands people and how to support them.