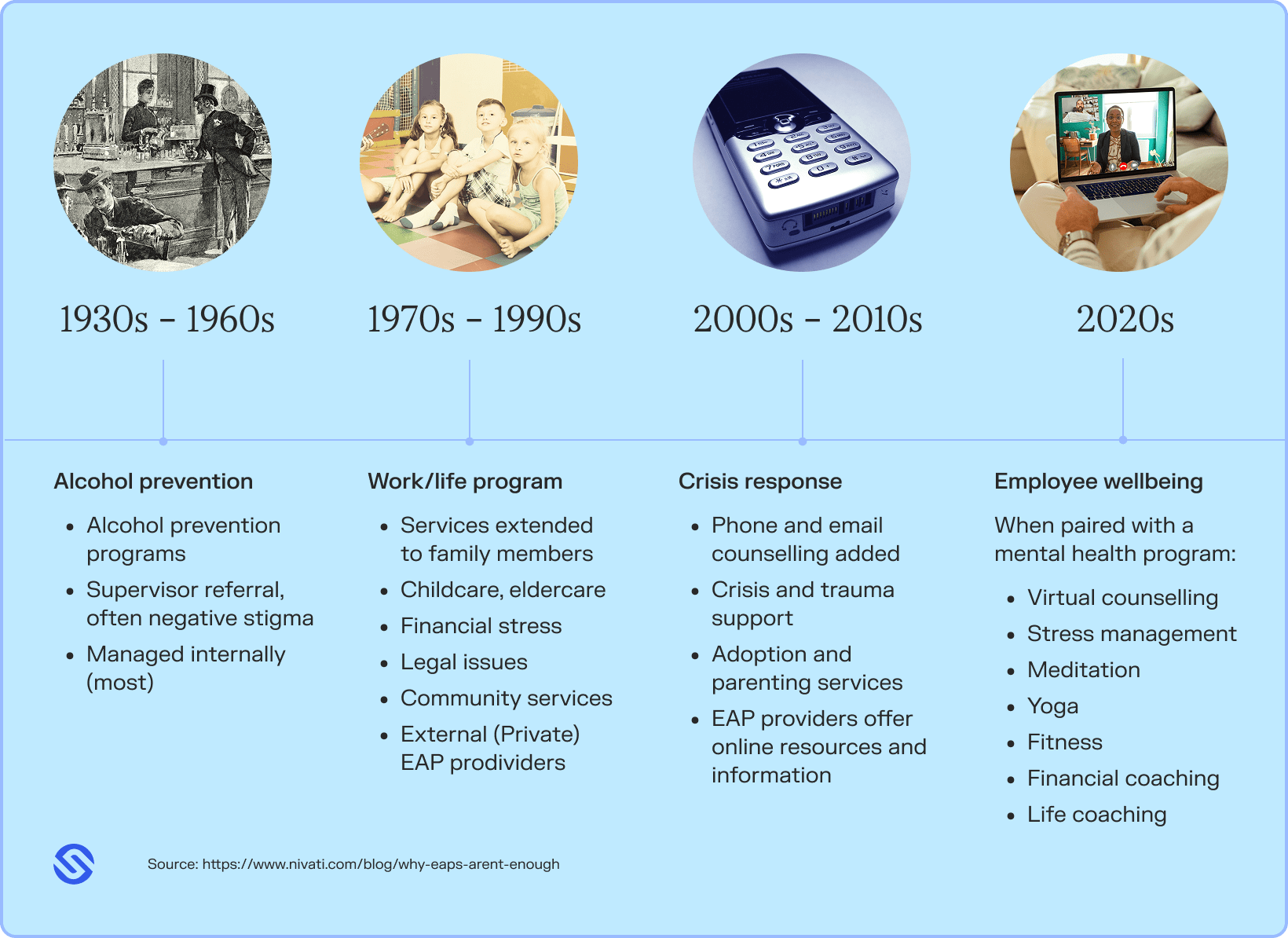
Traditionally, employee assistance programs (EAPs) were designed to help when an employee is already struggling. But unfortunately, they aren’t very proactive or focussed on long-term solutions. By the time an employee actually reaches out to an EAP service, their situation has often escalated to be far worse than it would be if the employee had timely, preventative healthcare access.
Employees need holistic, 24/7 access to medical and mental health professionals so they can seek health advice and treatment whenever they need it. This means issues won’t escalate, and they won’t have to take more time off work than needed. This approach empowers both employees and organisations, and is the smartest way to build a workplace wellbeing strategy.
In this article we’ll explore the history of EAPs, how different cultures approach them and why mental health can’t be treated in isolation. We’ll conclude with how modern solutions are offering a more effective way to manage employee health.
The limitations of EAPs
EAPs have been around for many years. As mental health challenges spread wider across the population, we are starting to see the limitations that come with EAPs. Let’s take a look at some of the limitations of today’s traditional EAPs.
EAPs have a cap on the number of sessions
Many types of EAPs can offer a narrow level of service. Unfortunately, many programs offer only a limited number of employer-funded sessions per employee, making it difficult to get to the root of the problem or move beyond quick wins and short-term fixes.
Typically, EAPs offer about three to six sessions per employee per year. Because of this limited time together, sessions can feel quite impersonal, and a one-size-fits-all approach is generally used.
“It’s not as simple as hey, here’s your counselling session. Most individuals need multiple pathways. It’s going to be very different based on what’s happening in each individual’s own personal life, their work and their family dynamics. It’s important to understand how complex people are and to not lead with a one-size-fits-all approach.”
Leanne Naber
Senior Account Executive at Sonder
As a result, many employees will decide not to proceed with follow-up sessions if they can’t afford it. This leads to the initial problem not being resolved, and in some cases, employees walk away feeling worse than when they started.
Many psychologists theorise that it takes more than twelve sessions to start seeing progress in a patient. As expected, long-term therapy is much more effective than short-term treatment for many wellbeing concerns, including mental health issues.
Stigma around mental health in the workplace
Although huge strides have been made in the mental health space, there is still a lot of stigma around mental health in the workplace. Seeking support for mental health issues can be daunting for employees, as there is typically a fear of being treated differently. Factors like fewer employment opportunities and promotions can come into play here, and this can prevent employees from seeking the help they need.
Another factor that can make employees less likely to seek this support is having to go through their internal HR team. Because of the stigma surrounding mental health in the workplace, people can feel embarrassed about having to voice health issues with fellow employees—which explains part of the reason EAPs are underutilised or difficult to access.
EAPs usually focus on short-term solutions
Because of the limited sessions available, it’s often difficult for EAPs to put preventative measures in place in terms of mental health and wellbeing. It is more likely that EAPs will intervene when issues are at a crisis point, which makes it hard to prevent problems from arising in the first place.
Instead of a holistic, early intervention strategy that helps to prevent mental health issues, or making a longer-term plan to manage an employee’s mental well-being, EAPs generally have more of a “band-aid approach.” This means patients must continue to book more time with a health professional to treat their concerns, which isn’t often possible in cases where their sessions have reached the limit.
How other countries look at traditional EAP services
EAPs are used all over the world, but the way they are utilised differs between each country.
In the United States, 81% of employers use EAPs, however usage is currently less than 10%.
Studies show EAPs have the ability to save money for organisations by reducing employee burnout and reducing things like absenteeism and presenteeism. But unfortunately, many employees don’t know what support is available to them, or how to access it. For example, only 29% of employees in Southeast Asia reported being aware of having access to EAPs provided by their employers.
Employees in the UK face a similar story. Out of the 5% of employees who have utilised their EAP, 42% of these people have been rejected for the therapy they need. Although the number of employers offering EAPs is high in countries around the world, a lot of employees don’t even know the programs exist or don’t use them because of the stigma around mental health in the workplace.
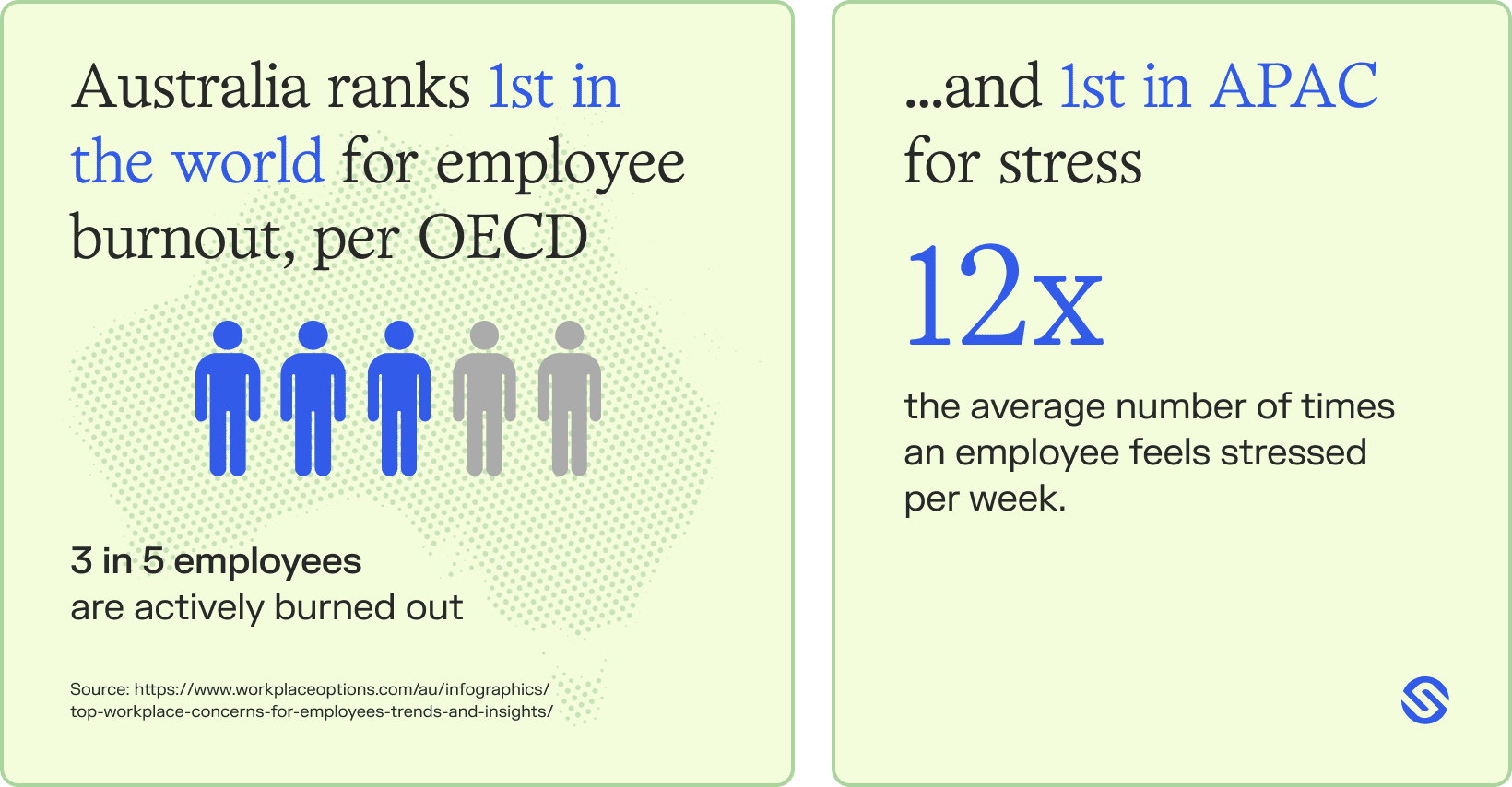
Closer to home in Australia, an estimated 80% of the top 500 businesses use EAPs, but the utilisation rates are very similar to those across the UK, US, and Southeast Asia. When assessing recent research*, the average utilisation rate of EAPs across Australia, the UK and the US tends to sit around 5%.
*References: IBISWorld, Productivity Commission, Society for Human Resource Management, The American Journal of Health Promotion, EAPA UK
The key differences in how other countries approach EAPs
Since different cultures operate differently, there are a few key differences in how EAPs are presented in workplaces globally. Factors like adapting programs to local values, such as how mental health is perceived in that location, or preferred communication style, mean that EAPs look different between different locations.
For example, North America offers more personalised care through EAPs, whereas many people in the UK and Australia reported that their care feels like a one-size-fits-all approach. Locations in Asia prioritise family values, and concerns about mental health stigma, which may make the programs more approachable for employees.
Other countries should take the lead from EAPs in Europe and Latin America, who both prioritise work-life balance and don’t rely solely on Employee Assistance Programs. Instead, companies in these regions integrate EAPs with a wider mental health and wellbeing strategy in the workplace.
The link between GP care and mental health
GPs are often the first port of call for anyone seeking support for their mental health. GPs can assess an individual’s mental health, provide initial support and then refer them to more specialised services if needed.
Getting access to specialised care (such as an appointment with a psychologist) can sometimes be slow and difficult, whether that’s because of long waitlists or high costs. When employees can’t get timely support, their mental health can deteriorate quickly, which makes it harder for them to function both at work and in their personal lives.
Over time, this can lead to social isolation, as many people withdraw from friends, family or colleagues out of exhaustion or embarrassment. The stigma around mental health also comes into play here. If an employee feels like they should be able to handle things themselves, they may delay seeking support.
Many mental health issues require a GP referral for Medicare-supported treatment.
RACGP
If an employee is dealing with mental health issues but doesn’t reach out for support, this can manifest as more sick days or lower productivity. This is why early intervention through GPs is so important. Without it, employees can end up worsening their condition, may not get the help they need and may end up needing extended time away from work, too.
Learn how virtual care is the changing the landscape of workforce wellbeing with our report on breaking the access block to primary care.
Why real-time healthcare access is the future
Employees encounter health and wellbeing issues at any time of day—not just within office hours. With 24/7 access to health professionals and GPs, employees can address their health concerns as they arise, helping to reduce stress and uncertainty.
Employee-funded access to healthcare services through a holistic platform (like Sonder) means no more waiting weeks for an appointment or taking time off work to see a GP or psychologist. Instead, employees can seek out medical advice and treatment exactly when they need it, preventing minor mental health issues from becoming significant.
This, in turn, minimises work-life disruptions and promotes a sense of security, where employees know that help is always available.
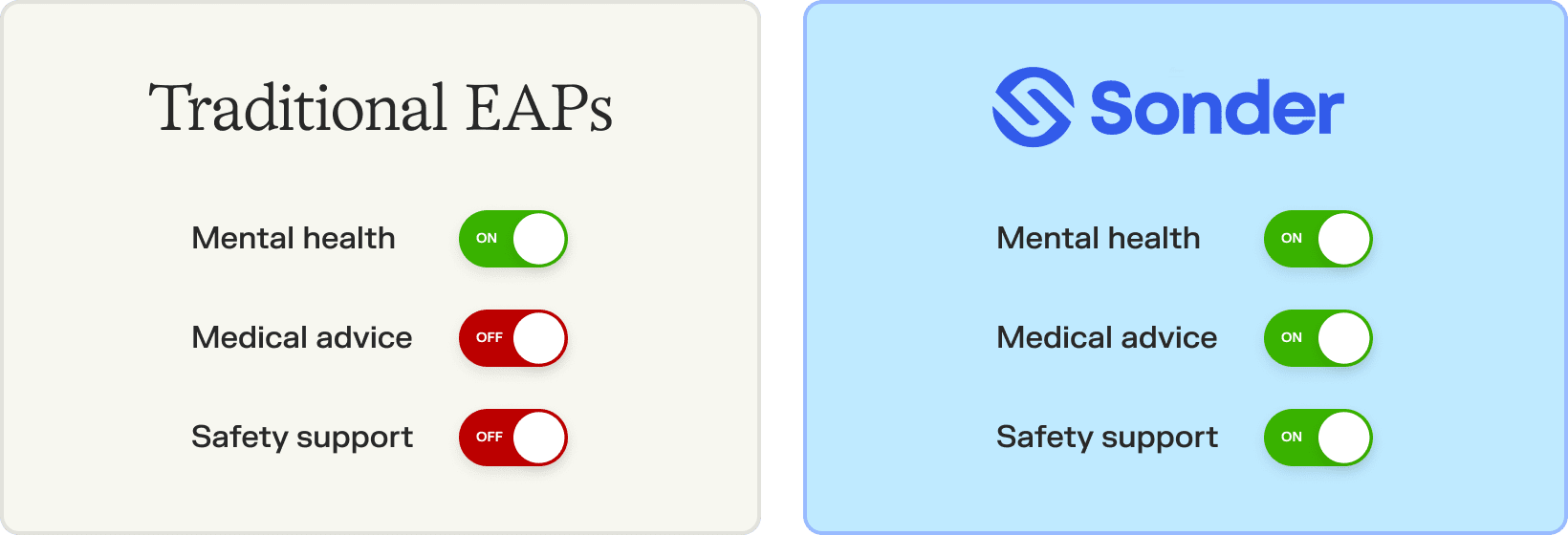
Unlike traditional EAPs, Sonder takes a proactive approach to healthcare that extends beyond mental health support alone. Our early intervention model isn’t only a hotline but a 24/7 always-on safety net, with trained professionals available real-time across all aspects of employee health—from mental health to medical support and even employee safety.
Employees don’t just get GP access, but also personalised health, wellbeing and safety tools and support tailored to them, from harm prevention tools to immediate, face-to-face support if they need it.
Here are some of the ways Sonders goes beyond traditional EAPs:
- No cap on the number of times employees can make contact with a health professional
- Receive immediate medical and mental health advice outside of business hours, anytime your employees need it through tools like Sonder GP Connect
- Anonymous and confidential service that employees can access from their phones without going through internal HR or other channels
- Peace of mind knowing that their mental health issues are private and won’t get back to their employer unless critical
- Preventative care and wellbeing strategy with a personalised self-help resource library available to employees
- Early intervention approach to injury management, with continuity of care and regular check-ins
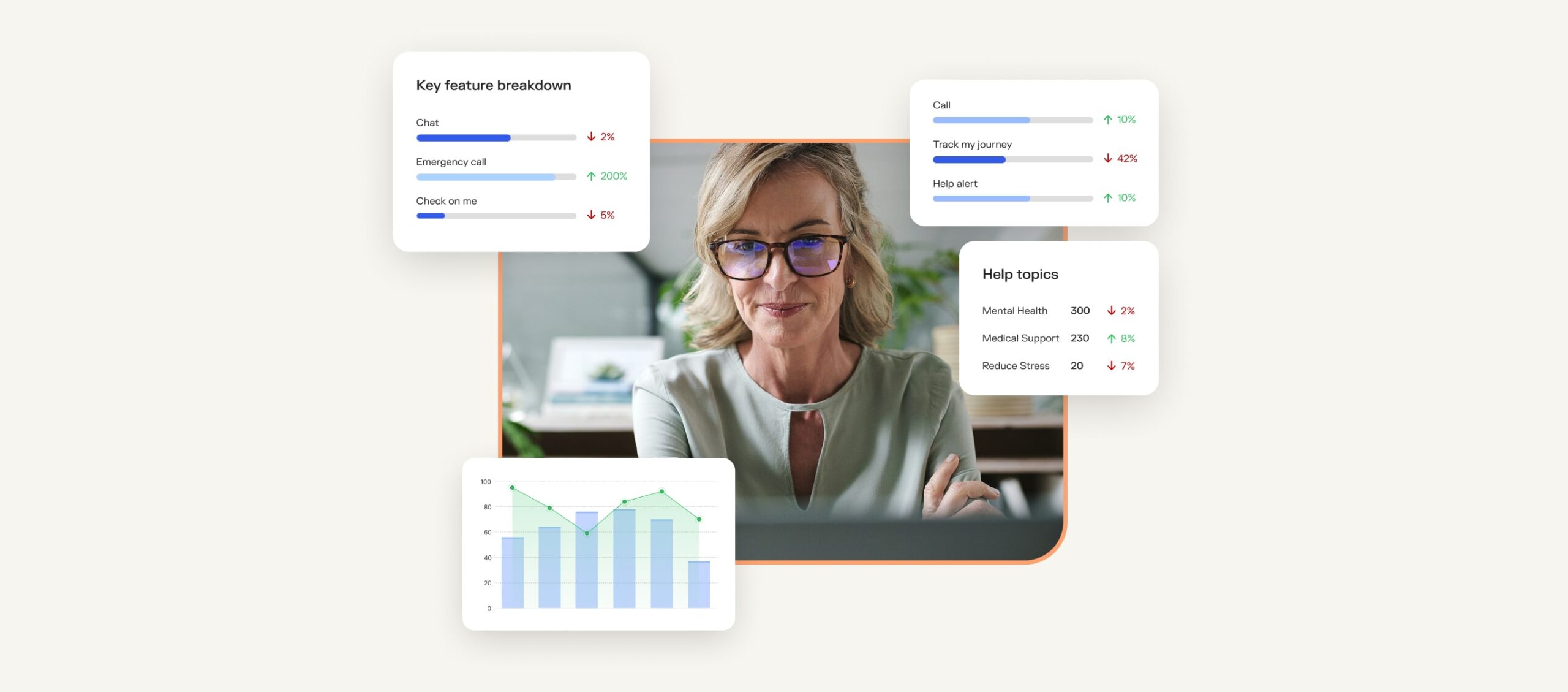
Sonder’s platform also offers real-time analytics that allows companies to assess the health and wellbeing of employees at all levels. From utilisation data to trends across entire teams, businesses can see where support is needed and make better-informed decisions about workplace wellbeing strategies.
Reassess your workplace wellbeing strategy
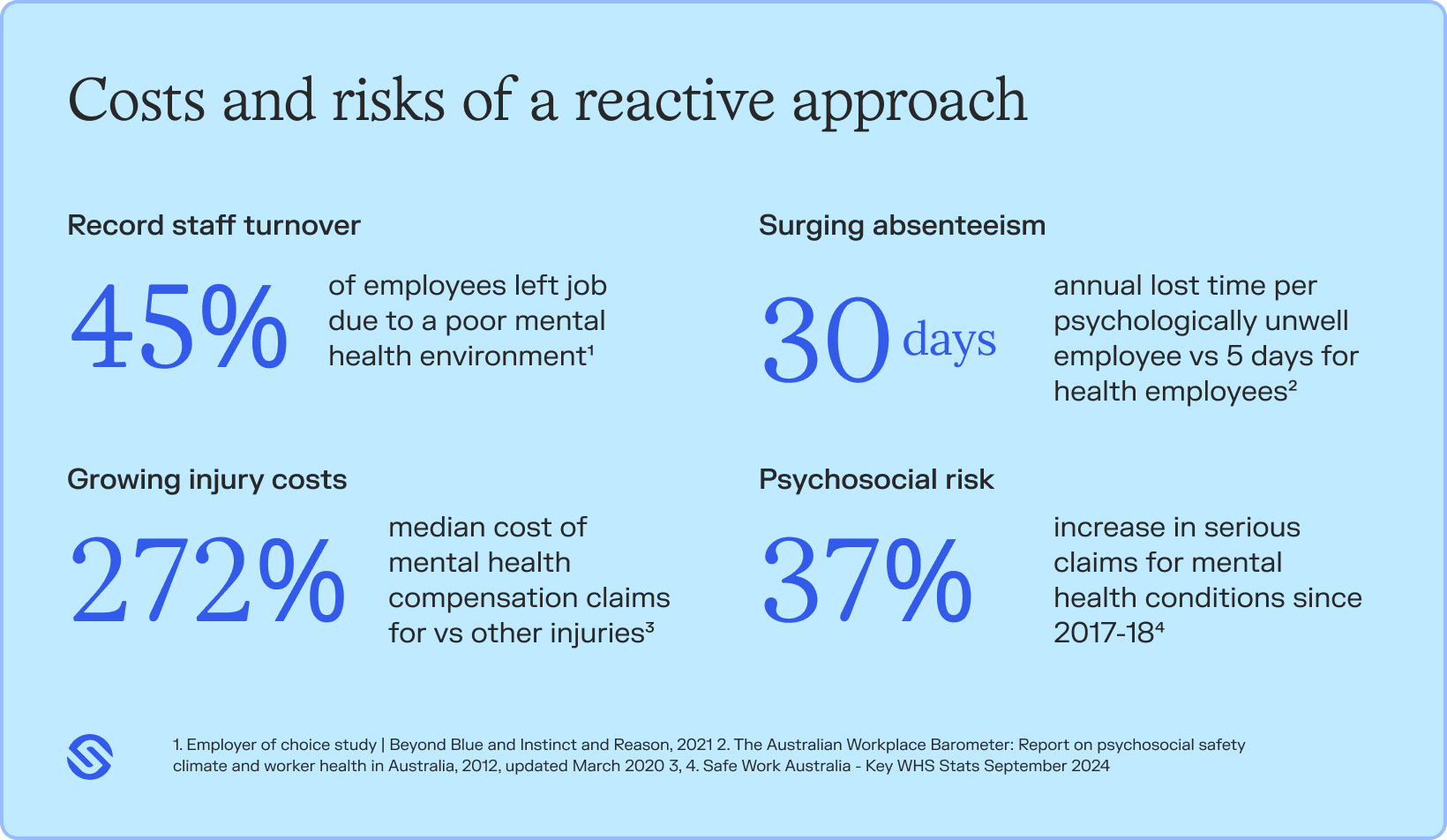
It’s time to re-think your workplace wellbeing strategy and move past outdated and reactive approaches to wellbeing among your employees. Employees need real-time, proactive support that makes them feel empowered and secure.
Investing in 24/7 healthcare access, harm prevention tools, and real-time insights is essential for a productive and resilient workforce. Try Sonder today and experience how 24/7 access to GPs and health professionals can help you build a thriving, engaged workforce.