At a glance:
- The access gap: Nearly 45,000 people in remote Australia have no access to a GP within a one-hour drive.
- The health risk: Regional residents are 2.5x more likely to be hospitalised for preventable illnesses due to delayed care.
- The business cost: Presenteeism from unmanaged health concerns costs the Australian economy $34 billion annually.
- The digital solution: Virtual care and telehealth bridge the geographical gap, delivering expert medical support in minutes, regardless of location.
Imagine waiting days for an urgent GP appointment. For Australians living outside metro areas, waiting upwards of 24 hours for urgent appointments is common.
28% of Australians (roughly 7 million people) live in regional, rural or remote areas. According to the Australian Institute of Health and Welfare (AIHW), Australians living in remote areas face several roadblocks when trying to access healthcare. Low population density, limited healthcare infrastructure, and the high cost of delivering care are just some of the reasons why Australia’s regional workforce is struggling to secure timely primary healthcare appointments.
But healthcare accessibility shouldn’t depend on where employees live.
By rolling out access to digital healthcare services (like telehealth), regional workers can secure the same level of care as their metro counterparts. Keep reading to discover how Sonder’s medical capabilities are bridging the primary care access gap and helping employees stay healthier, happier, and more productive.
What is the regional GP access block?
Booking a GP appointment is usually a straightforward task for metro employees. With plenty of medical centres and clinics located throughout capital cities and inner-city suburbs, receiving timely primary care is within reach.
But, it’s a very different story for rural and regional employees. According to the AIHW, reasonable access to primary healthcare means a person should be able to reach health services (like a GP) within a 60-minute drive time.
Unfortunately, data from the Royal Flying Doctor Service indicates this isn’t the case for Australians living in remote corners of the country. In fact, nearly 45,000 people in remote and very remote Australia have no access to any type of primary healthcare service within a one-hour drive of their primary residence.
“For Australians living in rural, remote and regional Australia, accessing simple services such as a nurse-led clinic, a GP, a dentist or a specialist is much, much harder.”
Frank Quinlan
Federation Executive Director of the Royal Flying Doctor Service
Many Australians in remote areas—notably regions of the Pilbara, Alice Springs, the Kimberley and Far North Queensland—have no access to essential primary healthcare, from GP appointments to general dental services and mental health support. As a result, these Australians are 2.5x more likely than metro residents to be hospitalised for a preventable illness or injury.
The regional GP access crisis in numbers
This is just the start of the healthcare access challenges facing regional Australians, which also include:
- Slow growth in regional GP numbers: Despite a 24.4% increase in the total number of medical practitioners from 2018 to 2023, the growth in GP numbers has fallen short of meeting the rising healthcare demands, especially in rural and regional communities. This shortage is only predicted to get worse, with a recent government report flagging there will be a shortage of over 5,000 GPs by 2033.
- Long wait times for urgent care: With fewer GPs located outside of major cities, over 50% of Australians in remote and regional areas are waiting over 24 hours for urgent GP appointments. Plus, 38% of outer-regional, remote or very remote Australians reported GP wait times as ‘unacceptable’, compared to just 28% of metro Australians.
- Limited access = poor healthcare experiences: Regional employees identified difficulty in booking appointments (47%) as the main reason not to recommend their GP.
- Regional GPs are overwhelmed with time-sensitive concerns: People located in regional or remote Australia are more likely than those residing in major cities to visit their GP for urgent medical care (9.1% vs 8%). This places additional strain on already stretched GP resources in remote and regional communities.
- Increased natural disasters: Regional and remote Australia is often prone to more extreme weather events, such as drought, flooding and bushfire. The Climate Council’s ‘On the Frontline: Climate Change & Rural Communities’ report finds the increase in extreme weather events is disproportionately affecting those in rural areas, with serious social, health and economic impacts. In terms of medical access, Australians in these areas are drastically impacted, with their physical access to care cut off.
What’s causing the primary healthcare access crisis in regional Australia?
So, where have these access issues stemmed from? There are several factors contributing to these healthcare access challenges, including:
- Low GP numbers in regional and remote areas: Research indicates that by 2028, remote communities will only have a fifth of the number of GPs compared to metro areas (43 compared to 255 per 100,000 residents).
- Incentivising GPs to move regionally is incredibly costly: Many country towns across Australia are resorting to offering six-figure salary packages and even free housing to attract city GPs out to the regions. If regional towns can’t afford to offer competitive incentives, the risk of being unable to attract or retain GPs rises.
- Regional communities need higher levels of healthcare support: With an ageing population and a higher incidence of chronic illnesses, regional communities need more GPs than metro areas. Unfortunately, that means that demand is currently outstripping supply for primary healthcare in regional areas.
- Medical graduates aren’t opting to pursue general practice: To compound the issue, just 10.5% of medical school graduates in Australia are listing general practice as their first choice specialisation. That means it’s becoming increasingly hard to fill job vacancies and solve the GP shortage in regional and rural Australia.
The GP access crisis in regional Australia boils down to this: fewer GPs, high demand for appointments, and long travel times to doctors’ clinics are causing remote and regional Australians to delay care or struggle to secure a timely appointment.
It’s not hard to see why this is leading to a lack of preventative care, meaning these Australians are experiencing higher rates of preventable hospitalisations, too.
The business risk of delayed healthcare
As a leader, you want to give your people the tools, resources and support they need to perform at their best. However, if your workforce is spread across regional and metro areas, there are important steps you need to take to ensure healthcare access is equitable and fair for your entire team.
If less unaddressed, the GP access gap that regional employees are facing can have a direct, measurable impact on your company culture and bottom line.
The longer staff go without timely healthcare, the more likely they are to face longer recovery times and extended periods away from work. Over time, this can lead to a rise in preventable injuries and illnesses and an even higher likelihood of employee turnover, too.
As a business, here’s what you risk by not addressing the regional GP access crisis.
A rise in preventable injuries and illnesses
Early intervention can help to lower the chance of preventable injuries and illnesses and even speed up an employee’s recovery, too. If a team member is navigating the early stages of a muscle strain or nasty flu, a timely GP visit can make all the difference in their recovery timeline.
Unfortunately, many companies are taking a reactive approach to injury management and healthcare. Australian businesses are facing $28.6 billion AUD in workers’ compensation costs each year due in large part to a fragmented system of care, administrative complexity, and a lack of accessibility for employees.
This issue is particularly pronounced for employees in regional areas. With fewer GPs and appointments available, addressing small health concerns before they become significant issues is difficult, leading to a rise in preventable illnesses as well as a spike in reactive care measures, such as seeking out care from an Emergency Department.
In 2022-23, there were 2.85 million presentations to emergency departments that could have been prevented by a visit to general practice.
RACGP
General Practice Health of the Nation Report 2024
An increase in absenteeism and presenteeism
Poor employee health can make it difficult for your people to do their best work. From chest infections to persistent migraines and other chronic health conditions, turning up to work while unwell is one key example of presenteeism.
While an employee might be physically at work, they’ll be unlikely to focus on the task at hand if they’re navigating pain, discomfort or poor physical wellbeing. For companies, presenteeism can spark a drop in productivity, a rise in ill-health among entire departments and even a decline in team morale.
In dollar terms, presenteeism has been estimated to cost the Australian economy $34 billion a year through productivity loss. Some studies suggest that presenteeism costs up to 1.7x an affected employee’s wage.
If left unchecked for long periods of time (which is often the case for regional employees waiting weeks to see their local GP), poor physical health can also lead to a rise in absenteeism. In Australian companies, absenteeism costs, on average, $3,500 per employee per annum, according to data from Direct Health Solutions.
A spike in employee turnover
The longer employees work while unwell, the higher their chances of needing to take extended leave to recover. With many regional employees facing challenges booking appointments and long wait times to see a GP, it’s very likely that members of your team may be working while navigating an illness or injury.
Again, the ripple effects of poor health and wellbeing are clear for employees and companies at large. Poor physical health can lead to poor mental health and a heightened chance of employee disengagement at work.
If your people aren’t given the resources and support they need to take care of their health, there’s every chance they move on to another company offering access to healthcare benefits or wellbeing services.
How digital healthcare bridges the gap
But waiting days or weeks to see a GP doesn’t have to be the reality for regional employees. Virtual healthcare (like telehealth appointments) breaks down the geographical barriers to accessing timely, personalised healthcare.
Rather than relying on doctors, GPs and specialists within a commutable distance of an employee’s home, telehealth allows your people to book virtual appointments with healthcare professionals, no matter where they’re located. With a wider pool of GPs within reach, regional employees can receive the same level of care no matter where they’re based.
“Telemedicine allows remote consultations, increasing accessibility. AI-driven tools aid in diagnosis and treatment decisions, offering insights from vast data sets. Wearable devices and health apps empower patients to monitor their health, promoting proactive care. Overall, these advancements save time, enhance accuracy, and enable more personalised healthcare, ultimately improving patient outcomes and the efficiency of general practice.”
RACGP
General Practice Health of the Nation Report 2024
While telehealth isn’t suited to all appointments, it’s a practical solution for employees who need to speak with a GP about their concerns, without the need for a physical examination. Plus, it ensures your employees can secure prescriptions and referrals while infectious, reducing the risk of spreading illness at work and in their community.
Sonder: Making healthcare accessible, no matter where employees are based
If you want to prevent a three-week recovery from becoming a three-month absence, it’s time to break down the barriers to accessing healthcare for your team in regional areas.
Sonder levels the playing field for regional employees. By providing 24/7 telehealth and safety support via a single app, we ensure that a worker in a remote mining town has the same immediate access to a doctor or mental health professional as someone in the CBD.
Plus, our triage process means employees can secure a telehealth appointment from a GP for things like minor ailments and ongoing conditions through Sonder GP Connect. From arranging blood tests to securing a referral to a psychologist, our telehealth offering allows your people to secure care without needing to wait for an in-person appointment.
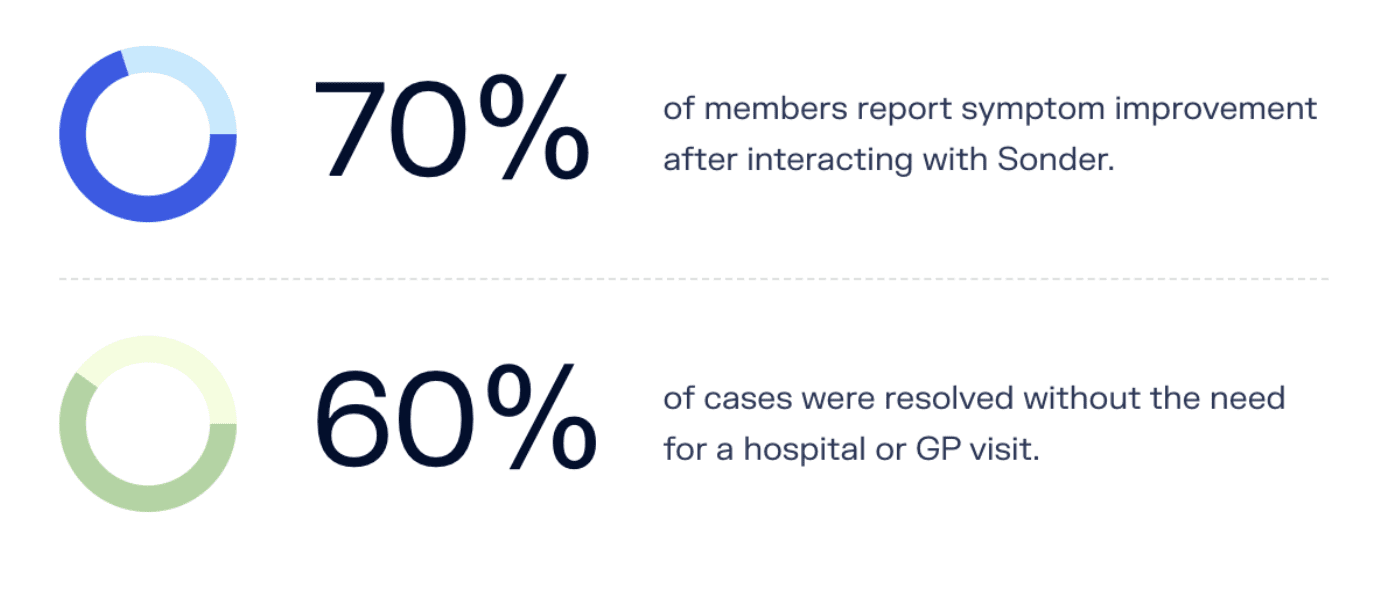
And the results speak for themselves.
Don’t let an employee’s postcode determine their healthcare access. Future-proof your workforce and give your people access to the care they need to reach their full potential.
Learn more about Sonder’s medical capabilities or see Sonder in action by requesting a demo.