At a glance:
- The $44 billion productivity drain: Poor GP access isn’t just a public health issue; it costs the Australian economy billions in lost productivity every year.
- The risk of presenteeism: When employees work while unwell because they can’t get an appointment, they often operate at just 50% capacity—increasing the risk of errors and burnout.
- Hidden WHS liabilities: Delaying medical care can lead to avoidable workers’ compensation claims and breaches in your duty of care.
- The 22% sick leave reduction: Providing 24/7 medical access allows for early intervention, which is proven to reduce unplanned leave and protect your team’s long-term health
To date, Australia’s primary healthcare access crisis has been framed as a public health issue. But in reality, it’s a growing business problem. Employees struggling to secure timely GP appointments are delaying essential care, leading to worsening health conditions, prolonged sick leave, and lower workplace productivity.
The data is alarming:
- 60% of Australians have delayed a GP visit due to cost or unavailability (Australian Healthcare Index, 2024).
- 246% increase in Australians postponing medical care due to affordability concerns (The Guardian, 2024).
- 37% of emergency department (ED) visits are for non-urgent conditions that a GP could manage (RACGP, 2024).
For businesses, this crisis manifests as higher absenteeism, increased presenteeism (a.k.a. employees working while sick or unable to perform at their best), and even long-term declines in workforce efficiency. The result is billions in lost productivity and rising employer healthcare costs.
But there are practical steps businesses can take to address this GP access crisis head-on.
What is the primary healthcare access crisis in Australia?
Visiting a primary healthcare practitioner, most commonly a GP, is becoming increasingly difficult and expensive.
There are many barriers to accessing timely care, from lengthy appointment wait times to high out-of-pocket costs and even a lack of bulk-billed appointments for GP visits.
While a $50 gap payment might be manageable for some, for others, it may be the reason they skip a GP appointment.
Dr Jamie Phillips, MB ChB, AFCHSM, DIMC, RCS(Edin), MRCGP(UK), FACRRM(EM)
Medical Director at Sonder
When we talk about the GP access crisis, we’re talking about the challenges Australians are facing when accessing primary care from their GP. As a result of growing costs and limited appointment availability, more Australians are delaying care, skipping appointments, and not getting on top of small issues before they become major health challenges.
Counting the costs of delayed healthcare for Australian businesses
When employees can’t access a GP in a timely manner, it doesn’t just affect their health – it directly impacts workplace productivity, profitability, and output at work.
In fact, delays in medical treatment can lead to prolonged sick leave, reduced performance, and even a heightened risk of staff turnover, too.
From rising absenteeism and presenteeism to the hidden costs of disengagement and turnover, poor GP access is draining billions from the Australian economy each year. For employers, failing to address this challenge can mean higher workforce instability, increased compensation claims, and preventable financial losses.
The growing cost of sick leave
Absenteeism is one of the most measurable business costs stemming from poor healthcare access. Employees who cannot access timely GP care often take longer to recover from common illnesses, leading to more frequent and extended sick leave.
Australian employees take an average of 10.5 sick days per year, costing businesses $3,500 per employee annually.
Absenteeism costs the Australian economy $44 billion per year in lost productivity.
Direct Health Solutions, 2024
Plus, workers with untreated chronic illnesses take, on average, two to three times more sick leave than those receiving early medical intervention.
How presenteeism impacts productivity
While absenteeism is a visible and measurable issue for businesses, presenteeism—when employees come to work while unwell—is often harder to spot, yet just as damaging. Employees who push through illness instead of taking time to recover may appear productive on the surface, but in reality, their ability to perform is significantly compromised.
Workers suffering from untreated illnesses, chronic pain, or fatigue often operate at just 50–60% of their usual capacity. Tasks that would normally take an hour might take twice as long, decision-making is slower, and the likelihood of mistakes increases.
In fast-paced industries like finance, retail, and logistics, these errors can have costly consequences—whether it’s financial miscalculations, incorrect orders, or workplace accidents.
Beyond individual performance, presenteeism can affect entire teams. Employees struggling with brain fog, exhaustion, or physical discomfort may inadvertently slow down collaborative projects, require additional oversight, or need work to be redone. This can increase the workload of other coworkers.
Worse still, in cases of contagious illnesses like the flu, employees who choose to “push through” often infect others, leading to secondary absences across the workforce and a cycle of reduced productivity.
For businesses, presenteeism quietly drains efficiency, impacts team morale, and increases the overall cost of lost productivity. Without timely GP access, minor health concerns can become long-term problems that affect entire teams—a hidden but serious risk for businesses striving to maintain operational efficiency.
The compliance risks of not addressing the GP access crisis
Beyond the costs and productivity impacts of absenteeism and presenteeism, businesses also face legal and compliance risks if they fail to ensure employees have access to timely healthcare.
Under Australian workplace laws, employers have a duty of care to protect their employees’ health and wellbeing. This includes proactively addressing preventable health risks and ensuring that workplace conditions do not contribute to worsening medical conditions or injuries.
Failure to meet these obligations can result in legal action, increased risk of workers’ compensation claims, and even reputational damage. As employees struggle with limited GP access, conditions that could have been treated early escalate into serious workplace health concerns, increasing the risk of compliance breaches.
Providing proactive healthcare solutions, such as GP telehealth access, can help businesses mitigate these risks by enabling employees to address health concerns before they impact their ability to work safely and effectively.
Workplace Health and Safety (WHS) compliance risks
Under Australian Work Health and Safety (WHS) laws, employers are required to take reasonable steps to protect employee health. This means ensuring that work-related risks are minimised and that employees have access to medical care when needed.
When businesses fail to address workplace health risks, they expose themselves to potential liability issues, legal disputes, and financial penalties. Some key compliance risks include:
- Employer negligence claims: If an employee’s health deteriorates due to inaccessible healthcare or delayed treatment, the company could face legal action for failing to provide a safe working environment.
- Increased risk of workers’ compensation claims: Employees suffering from untreated illnesses or workplace-related injuries may file claims for compensation, adding financial strain to the business.
- Higher compensation payouts: If employees are unable to receive timely GP treatment, minor health concerns can worsen into chronic conditions or serious workplace injuries, leading to expensive compensation claims and legal fees.
By ensuring employees have easy, employer-funded access to GP consultations, businesses can proactively prevent minor health concerns from escalating into legal and financial risks—while also fostering a safer, healthier, and more productive workforce.
Why providing 24/7 GP access is a cost-saving strategy
Businesses implementing telehealth solutions report at least a 22% reduction in absenteeism costs. But that’s just the start of what businesses stand to gain from rolling out an employer-funded GP telehealth service.
| The business case for offering 24/7 GP access via telehealth | ||
| Concern | Without GP Telehealth | With GP Telehealth |
| Average GP wait time | Four days | Same-day consult |
| Likelihood of condition worsening due to delays | High | Low |
| Average sick leave per employee per year | 10.5 days | 7.9 days* |
| Annual cost of absenteeism per employee | $3,500+ | $2,633 |
| Overall business productivity impact | High impact and severe drop in productivity | Lower impact and fewer productivity disruptions |
*This is an estimated figure based on modelling of reduction in an individual’s time to be seen by a healthcare practitioner, leave taken to see a primary care provider, time spent travelling to and from primary care. Based on international studies.
How businesses can take action
As the cost of absenteeism, presenteeism, and delayed healthcare access continues to rise, businesses must take a proactive approach to protecting employee wellbeing and improving productivity.
Implementing GP telehealth services isn’t just about offering an extra employee benefit—it’s a strategic move that can reduce workplace disruptions, lower healthcare costs, and boost overall employee engagement.
- Assess current workforce health trends
- Compare the costs of absenteeism vs. investing in GP telehealth
- Implement GP telehealth as a strategic employee benefit
To take meaningful action, businesses should start with the following steps:
1. Assess current workforce health trends
Begin by evaluating your company’s absenteeism and presenteeism rates. Look at the patterns of sick leave, the reasons employees are taking time off, and whether certain health conditions are becoming recurring issues.
- Are employees frequently taking extended sick leave due to minor illnesses that could have been treated sooner?
- Are some team members showing signs of presenteeism, working while unwell and underperforming as a result?
HR teams and business leaders can gather insights by reviewing internal sick leave data, conducting employee wellbeing surveys, and tracking productivity fluctuations. Identifying these trends will provide a clear picture of the impact poor GP access is having on your workforce.
2. Compare the costs of absenteeism vs. investing in telehealth
Once you understand your workforce health trends, quantify the financial impact of absenteeism and presenteeism. Consider:
- How much is your business losing annually due to sick leave?
- What are the indirect costs, such as lost productivity, overtime pay, and workflow disruptions?
- How often are employees delaying GP visits due to cost or accessibility issues, leading to prolonged absences?
Then, compare these costs to the investment required for implementing virtual care services. Many businesses find that the return on investment (ROI) from reducing absenteeism and presenteeism far outweighs the costs of providing telehealth access.
3. Implement telehealth as a strategic employee benefit
With 86% of Australians visiting a primary healthcare provider at least once a year, offering discounted access to these services is a valuable perk that sets your business apart. Investing in your team’s health this way boosts retention and engagement by providing a benefit they’ll actually use.
After identifying the business impact, the next step is integrating telehealth into your employee benefits package. By offering 24/7 access to GPs through a dedicated employer-supported telehealth service, employees can secure prescriptions, general medical advice and specialist referrals quickly.
By offering GP telehealth to teams, businesses can ensure that employees receive timely medical care without long wait times or financial barriers.
How Sonder’s GP and medical services can help employers act now
For many businesses, employee absenteeism and declining productivity aren’t only HR challenges, they’re direct results of poor healthcare accessibility. Long wait times for GP appointments, high out-of-pocket costs, and limited bulk-billing options often lead employees to delay seeking medical care, which can turn minor health issues into major workplace disruptions.
Here’s how Sonder’s virtual telehealth and medical services are helping businesses take control of employee health outcomes and create a more resilient, high-performing workforce.
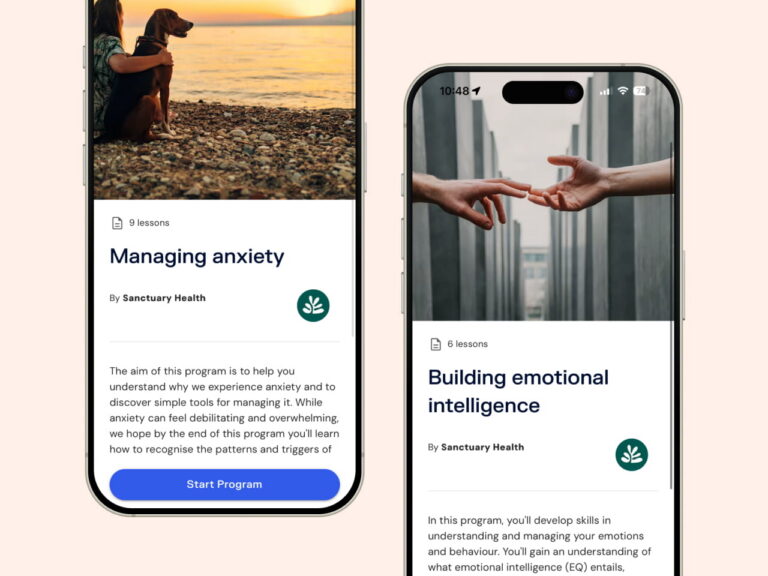
Immediate medical consultations without the wait
Accessible 24/7, Sonder’s early intervention approach ensures employees can get immediate expert medical advice from our emergency-qualified nurses to improve recovery outcomes and reduce lost time. Our nurses can conduct a clinical assessment within minutes and triage employees to the appropriate treatment.
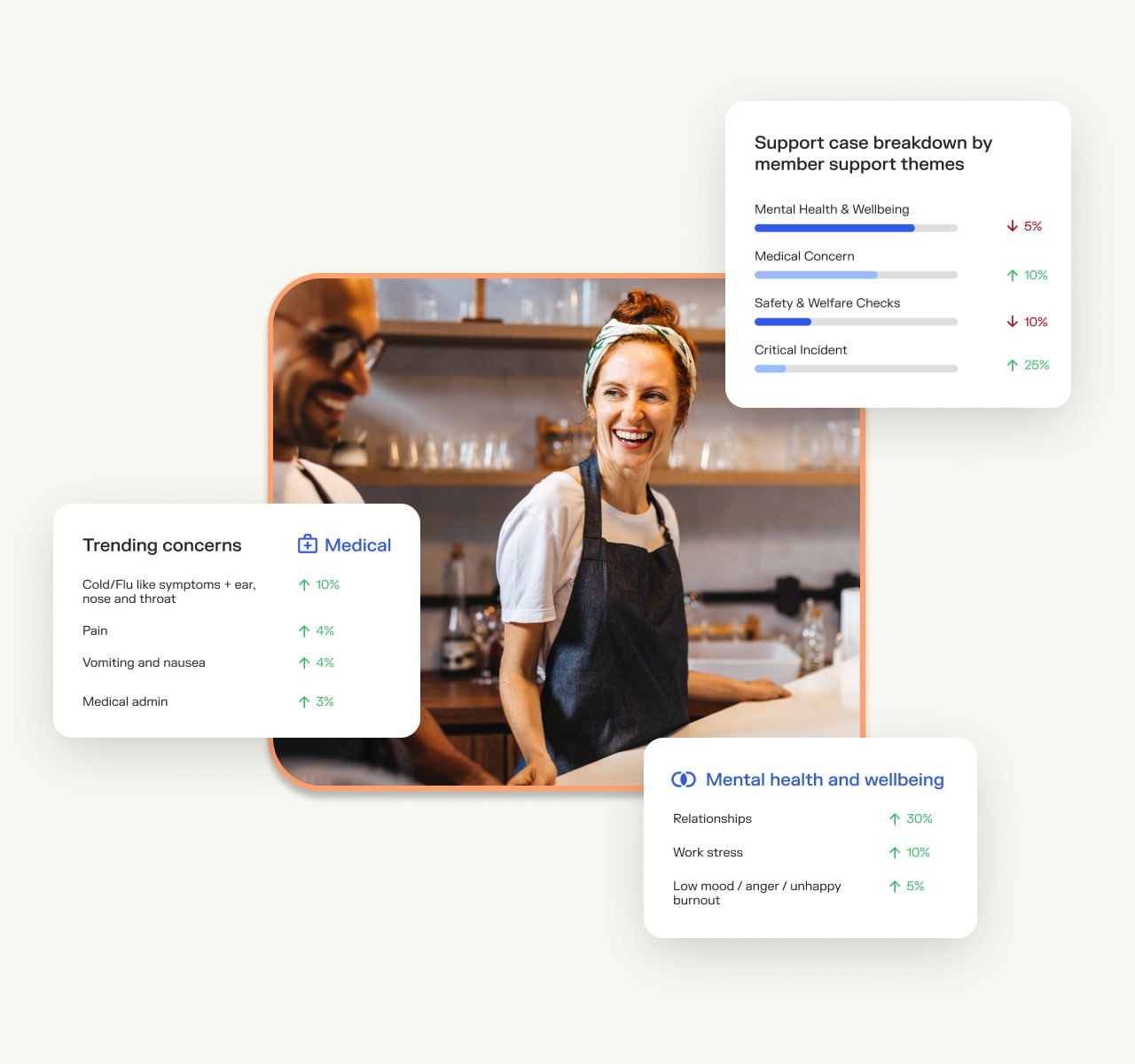
Data-driven workforce health insights for HR leaders
Sonder’s corporate health dashboard provides HR teams with real-time insights into workforce health trends, absenteeism patterns, and areas for proactive intervention. By identifying recurring health issues, businesses can implement targeted wellness programs and improve employee health outcomes.
Timely access to GP telehealth appointments
With Sonder, employers can offer a range of medical services to employees including telehealth GP consultations through Sonder GP Connect.
Using the Sonder app, employees can connect with registered nurses to self-manage their symptoms or find out which over-the-counter medication is right for their needs. From there, nurses might help employees set up telehealth appointments with a GP, helping to remove barriers to accessing care.
Through telehealth consultations, GPs in Sonder’s network can issue prescriptions, allowing employees to access medication without the need for an in-person visit. This service streamlines healthcare access, particularly for those managing chronic conditions or dealing with common illnesses.
By removing critical blockers to medical care, we can help your people stay healthier, happier, and more productive. This streamlined experience offers cost savings, reduction in lost time, simplified medical access, and ensures the right care is delivered at the right time to your people.
Take action today
Sonder bypasses the “access block” by providing 24/7 on-demand clinical triage. With 57% of our support cases occurring after hours, we ensure employees get professional medical advice when traditional GPs are closed, reducing preventable absenteeism.
Companies that prioritise employee health see measurable improvements in productivity, retention, and workplace morale. Investing in proactive, accessible healthcare solutions today can prevent significant financial and operational losses in the future.
For a deeper analysis of how GP telehealth can transform your workforce, download the Breaking the access block report now.
Ready to see Sonder’s features in action? Try it now and see for yourself.