At a glance:
- Connection over correction: You don’t need to be a counsellor to support a colleague; what matters most is listening without judgment and being fully present.
- The power of validation: Research from the Black Dog Institute shows that feeling heard and validated significantly lowers psychological distress.
- Avoid the “accidental counsellor” pitfall: Supporting someone doesn’t mean carrying their pain—it means acting as a trusted first point of contact to help them navigate their next steps.
- Proactive support: Moving from a simple check-in to genuine care involves consistent follow-ups and knowing when to bridge the gap to professional help.
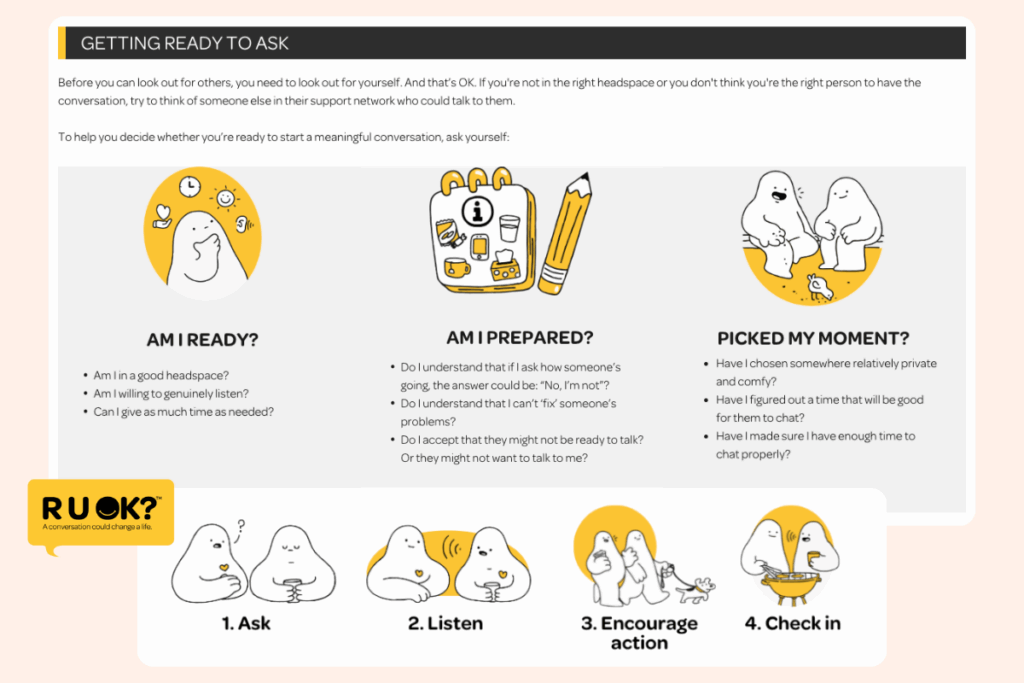
As R U OK? Day approaches, it’s a timely reminder that checking in with your team is an ongoing part of building a supportive and effective workplace.
As a team leader, you’re often the first to notice when someone isn’t themselves: perhaps they’ve been quieter than usual, seem easily frustrated, or just don’t feel like their usual self. Those little changes often stand out and can be the first sign that someone is struggling beneath the surface.
The good news is, you don’t need to be a counsellor or have all the answers. What matters most is being the one to take that first step: choosing a good moment, asking the question, and listening without judgment.
Sometimes, the conversation will be short and simple — a reassurance that you care, and that support is there if they need it. But other times, your people may say, “no, I’m not okay.”
That’s when your role shifts from just checking in to guiding them toward the right support in a way that feels safe, proactive and respectful.
Disclaimer: The information contained in this article and on this website is general information only and does not constitute legal advice. Although all efforts have been made to ensure the accuracy and currency of the information presented, Sonder takes no responsibility for any errors or omissions presented. Please contact a legal representative for individual advice.
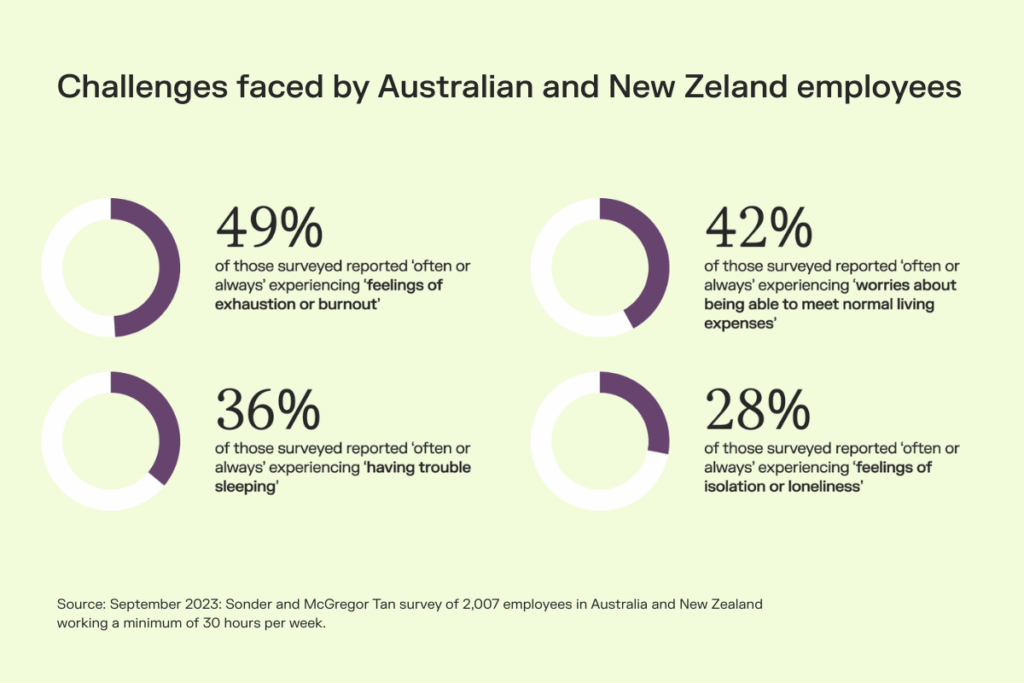
What the data tells us about workplace mental health
For many employees, admitting they’re not okay is an incredibly hard thing to do. In fact, more than half of Australian workers (53%) say they’re hesitant to talk about their mental health at work. That means if someone does open up to you, it usually means it’s taken them a fair bit of courage to do so, and it’s important to be prepared for the moment.
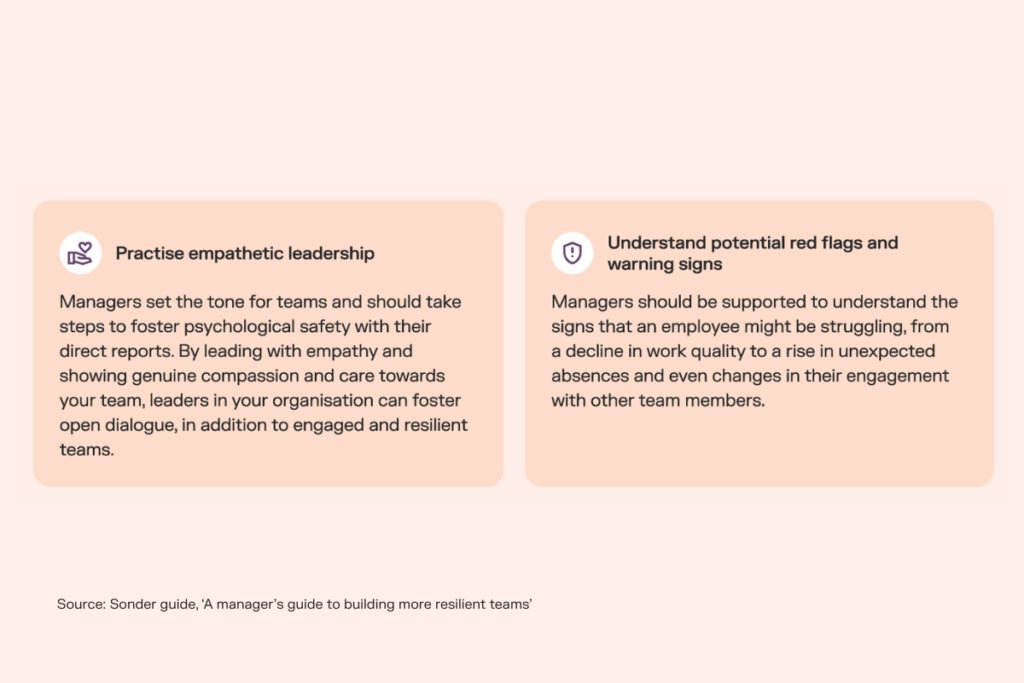
Research shows that managers hold enormous influence over how people experience their wellbeing at work. In fact, they can impact mental health just as much as a spouse (69%), and even more than a doctor (51%) or therapist (41%). And yet, only around half of employees (55%) feel safe bringing their mental health concerns to their manager.
This gap highlights how having a good working relationship isn’t always enough. Employees need to feel confident that if they say, “no, I’m not okay,” their manager will handle that moment with sensitivity and empathy.
That’s why what happens next matters just as much as asking the question in the first place. So, what do you do if the answer is “no”? Let’s take a closer look.
How do I respond if someone says they are not okay?
It’s natural to want to try to help “fix” things as soon as someone shares a struggle. But more often, what a person needs first is simply to be seen and heard.
Here’s a checklist of how to show up and create a safe and supportive space as an immediate response. Be sure to bookmark this one for later.
✅ | Avoid rushing solutions | Jumping in too quickly with solutions can stop a person from fully exploring their thoughts, unintentionally minimise their experience, and even obscure the root of the issue. Taking the time to listen, acknowledge, and validate what they’re going through can be far more supportive than offering advice right away. |
✅ | Listen without judgment | During these conversations, be sure to give someone your full attention and let them speak without interruption or evaluation. Meaningful listening also requires you to get comfortable with silence — giving them space to gather their own thoughts without input, whilst showing you’re truly present. Gentle cues like “I see” or “mhmm” can reassure them you’re listening without judgment. |
✅ | Stay present in the moment | Make time for an uninterrupted conversation, free from calls, notifications, and watching the clock. Even small disruptions can make someone in a vulnerable situation feel unseen and close off. Being fully present helps build psychological safety, showing that you genuinely care and allowing them the space to open up without feeling rushed or dismissed. |
✅ | Acknowledge their trust | When someone opens up, reassure them that their words are confidential and respect that trust by protecting their information. This doesn’t mean you need to act as an ongoing “accidental counsellor” — rather, you can be a trusted confidant and a first point of contact to help connect them with a listening ear, followed by the right support if needed. |
What not to do — common pitfalls to be aware of
Even with the best intentions, it can be challenging to know the right way to respond when someone is struggling. Sometimes, in trying to help, we unintentionally make things harder.
The following are some common mistakes to be mindful of when having these kinds of conversations:
❌ | Minimising their experience | Sometimes, in an attempt to help, we may try to reassure someone that it’s “not such a big deal.” Even with good intentions, this can make them feel misunderstood, dismissed, or as if there’s something wrong with them. Everyone’s emotions are valid, and it’s not up to us to judge their significance. Instead, lean on listening statements like: “I hear you,” “That sounds really hard,” “It’s understandable you feel that way,” or “What you’re feeling is valid.” |
❌ | Offering unsolicited advice | Many well-meaning people offer advice, thinking they are helping, but it can often be received very differently. Giving advice unasked can feel condescending, like criticism, or take away their sense of autonomy. We all value having control over our own lives, which is why it’s important not to assume we know better. Instead, focus on listening and asking open-ended questions that help them remain actively engaged in a conversation about themselves. |
❌ | Making it about your own experiences | While it can feel like a good way to relate, sharing your own story can sometimes shift the focus away from the person who is struggling. Even with the best intentions, it may discourage them from staying vulnerable. Instead, ask thoughtful questions like: “How have things been since then?” or “What’s been the hardest part for you?” This keeps the conversation centered on them and gives them the space to explore what matters most. |
❌ | Promising confidentiality you can’t keep | Building trust means being honest about your limits. If a conversation requires involving your manager, HR, or mandatory reporting (for example, if there are concerns about self-harm), explain this gently and clearly. Let them know what will remain confidential and why additional support may be needed. Transparency helps maintain trust while ensuring they get the help they need. |
Practical steps towards additional support
Once you’ve given someone the space to share openly, listened without judgment, and shown that you are fully present, you can gently guide the conversation toward practical support.
Again, the aim is not to “fix” everything, but to help them access the resources and reassurance they need.
Here are four practical steps to take:
- Ask what they need right now: Start by checking in with them directly. Simple questions like “What would be most helpful for you right now?” or “How can I support you today?” put the focus on their needs and give them agency.
- Connect them to professional resources: Ensure they know where to turn for expert help, whether that’s an Employee Assistance Program (EAP), an alternative like Sonder, counselling, or other support services. Offering guidance in a calm, non-pressuring way shows you care without overstepping.
- Follow up consistently: Support doesn’t end after one conversation. Regular check-ins, whether brief messages or in-person catch-ups, demonstrate that you genuinely care about their wellbeing and are there for ongoing support.
- Know when to escalate: Some situations may require additional support, such as HR involvement or mandatory reporting (for example, if there are concerns about self-harm). Be transparent about this if it arises, explaining why it’s necessary while reassuring them that their privacy is respected wherever possible.
With psychosocial regulations now in place, it's crucial that businesses not only recognise these issues but also equip their employees with the tools and support needed to raise concerns and seek help effectively.

Chief People Officer at Sonder
When to move from peer to professional support
It’s natural to want to support your team members through challenging times. However, it’s essential to recognise the limitations of peer support and when professional help is necessary.
Signs that someone needs more than a chat
Keep an eye out for these warning signs that can signal deeper mental health struggles and where professional help is needed:
- Persistent sadness or mood swings: They may seem unusually quiet, tearful, irritable, or experience noticeable shifts in mood during the workday.
- Withdrawal from social interactions: Avoiding team discussions, skipping lunch or coffee breaks, or disengaging from usual collaboration.
- Changes in work performance: Missed deadlines, frequent mistakes, difficulty concentrating, or reduced participation in meetings.
- Physical symptoms at work: Appearing unusually tired, complaining of headaches or other aches, or showing low energy.
- Expressing hopelessness or worthlessness: Making statements like “I can’t keep up” or seeming disengaged from responsibilities and team goals.
For more warning signs to look out for, check out the official ‘How to ask R U OK? at work’ guide — you may even consider printing it out for the wider team.
How to make a referral in a supportive way
It’s not uncommon for team leaders to become accidental counsellors — but this can lead to burnout, as senior leaders aren’t trained to provide the level of mental health support that professional counsellors can offer. That’s why it’s important to make the right referrals at the right time.
Line managers are not mental health experts
Referring someone, however, can sometimes feel like sending them from one support service to another. So how can we approach this process with sensitivity and care?
- Initiate the conversation with empathy: Express concern and support, emphasising that seeking help is a positive and courageous step.
- Provide information: Share details about available resources, such as Employee Assistance Programs (EAPs), an alternative like Sonder, or local mental health services, to empower the individual with choices.
- Offer assistance: If appropriate, help them make initial contact or help plan their workload around appointments, showing that you’re there to support them through the process.
- Respect their autonomy: Understand that the decision to seek help is personal. Offer support without pressuring, and respect their pace and choices.
Bridging the gap with support for your whole organisation
R U OK? Day is a timely reminder that asking someone if they’re okay can be the start of a crucial conversation — but what happens next is just as important.
In the workplace, research shows less than a quarter of employees (24%) feel comfortable discussing mental health with HR or management, while over two fifths (44%) feel at ease speaking with a Mental Health First Aider. This highlights the importance of having trained, approachable professionals available and the need for clear pathways so employees can access support that feels safe and trusted.
Sonder bridges the gap between that first question and ongoing care by offering guidance and 24/7 access to qualified professionals. Support is available not only for employees but also for the leaders who are supporting them.
Quite often employers forget that because an individual has ‘manager’ or ‘supervisor’ in their title, they don’t actually know how to manage or to deal with all situations. At Sonder, we support the manager, ensuring they can still do their normal role, but more importantly, be there for that manager to lean on for support when they need it.

Head of Member Safety at Sonder
Sonder’s resources complement, rather than replace, human connection, providing guidance, advice, and ongoing check-ins so crucial moments aren’t missed, even amidst busy workloads. And if you’re ever unsure what to do next, there’s always someone to call.
With tools, guidance, and support structures like Sonder, organisations can ensure that employees are not only asked the right questions but also receive timely, compassionate follow-up. By putting these systems in place, workplaces can build a culture where people feel truly seen, heard, and supported — every day, not just on R U OK? Day.
Try Sonder today and experience how 24/7 access to safety experts, mental health and medical professionals can help you build a supported, healthy workforce.
Want to hear more on what to say when someone’s not okay? Watch Sonder’s webinar on “What to say when someone says they’re not OK” and hear from the experts.
If you or someone you know needs help, call:
- Emergency on 000 (or 112 from a mobile phone)
- Lifeline on 13 11 14
- MensLine Australia on 1300 789 978
- Suicide Call Back Service on 1300 659 467