At a glance:
- Measurable outcomes: Transitioning to a connected model of care reduces the escalation of minor issues into crises, lowering absenteeism and improving the ROI of wellbeing investments.
- The fragmentation trap: Most organisations invest in multiple wellbeing services, yet employees often fail to use them because the pathways to care are overwhelming and unclear.
- Simplicity as a safety net: A single entry point removes the “burden of diagnosis” from the employee, allowing them to seek help without needing to interpret a complex system.
- The trust catalyst: Employees are more likely to seek help early when they engage with a platform that is proactive, confidential and human-led.
You’ve got all the right intentions, you’ve provided a range of support services, and yet, your people aren’t using them. This can be incredibly frustrating. You were told that investing in wellbeing would cause an increase in engagement, productivity and lowered turnover and absence. But instead, your team seems more passive than ever, unexpected absences are climbing and finance is following up about all the underutilised services. This isn’t an uncommon experience, and fragmented support certainly doesn’t help.
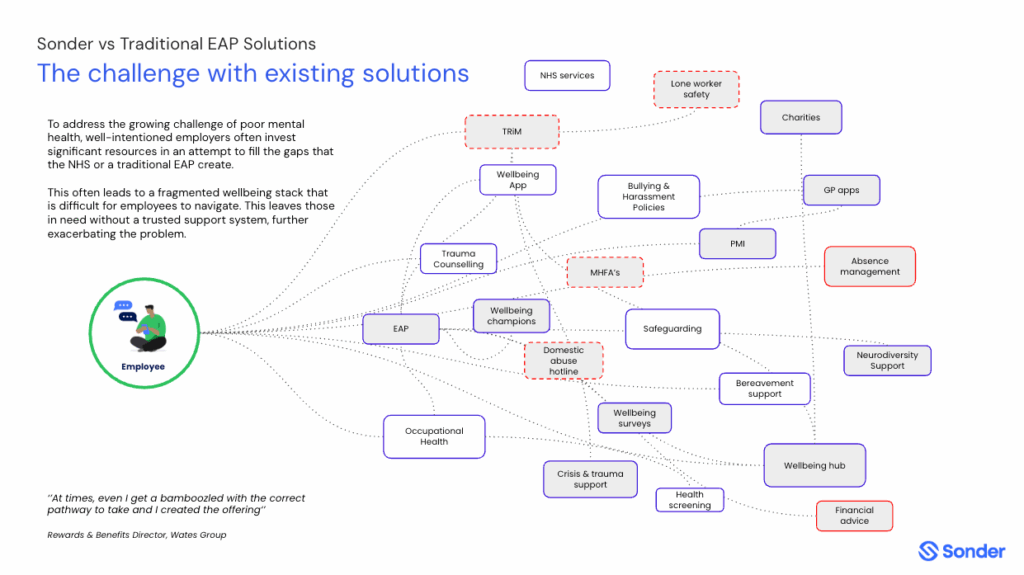
Across the UK, organisations are investing heavily in the wellbeing of their people. Mental health support, medical helplines, financial coaching, on-demand GPs, safety tools, occupational health, private medical insurance and peer networks all play a role. Each service is created with good intent. Yet when someone actually needs help, the experience of accessing support can feel complicated and unclear.
This disconnect between someone needing support, but failing to access it isn’t because support isn’t available, it’s because the provided systems are overwhelming to navigate and challenging to engage with. This is made worse by stress, physical symptoms, pain, fatigue or personal concerns that overlap. In these moments, confusion leads to hesitation. People wait, hoping things will improve, and challenges that could have been addressed early become more serious over time.
When support exists but is hard to reach
Think of your wellbeing model like this: Imagine you’re doing your weekly grocery shop. You’ve had a really long day, you’re tired, and you’ve forgotten your list. Perhaps you even have restless kids in tow—it’s already a lot. Then, you find there are no Tesco, Asda, or similar all-in-one supermarkets. Instead, you have to travel all over town to hunt down every single item separately. It’s more than likely one place you needed is closed, and another doesn’t even have the item you need. What a nightmare! Of course, this isn’t a perfect analogy for care; many people prefer specific destinations like the local baker, butcher, and greengrocer. However, if someone is in urgent need and hasn’t had the time to plan, you can see how a one-stop-shop becomes the difference between getting your week sorted and having a meltdown that ends in a takeaway box of pad-thai.
When someone is doing well, they may be able to stay on top of the different elements of their wellbeing. They know exactly what they need and how to access separate services. However, in those critical moments of distress or urgency, fragmented support can create barriers to care. On an already overloaded brain, the paradox of choice results in decision paralysis.
This pattern is common across industries. Even wellbeing leaders, HR professionals and managers who understand the system can find it difficult to articulate where each pathway begins and ends. One rewards and benefits director from a UK construction company put it plainly: “Even I get confused about the correct pathway to take, and I designed the wellbeing offering.”
Employees are often expected to diagnose their own needs and match them to the correct service. This is a lot to ask of someone who is already struggling. When people are unsure, they delay reaching out. As needs escalate, the personal impact becomes more serious and the organisational cost rises. Stress becomes burnout. A medical question becomes avoidable treatment. A safety concern becomes an incident. Not to mention, that this sort of approach can result in the whole picture being missed.
This is not a failure of intent, investment or care. It is a design challenge.
A more human starting point
When someone’s wellbeing is stable, they often have the capacity to coordinate various services and find what they need. But when they are facing distress or urgency, requiring them to navigate multiple, separate care elements is too much. A single entry point transforms from a convenience into a critical safety net that stops a crisis from escalating.
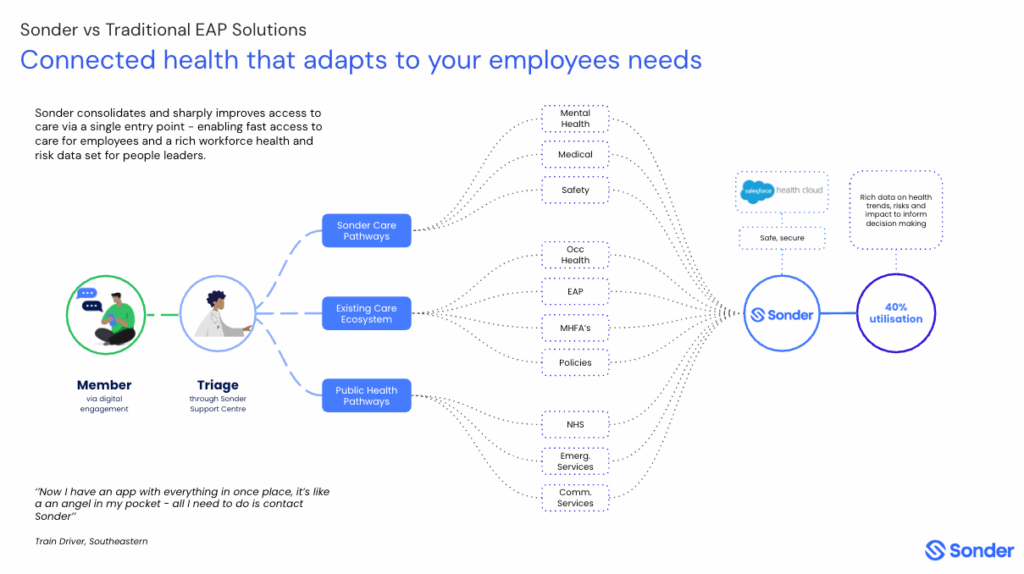
Instead of multiple entry points, organisations can provide one trusted place to start, no matter what the issue relates to. From this single entry point, trained support professionals can understand what is going on and guide the individual to the right form of help, whether it’s mental health support, medical advice, safety assistance, workplace processes or specialist care.
The individual does not need to interpret the system. They do not need to decide what is “appropriate enough” to seek support for. They simply begin, and the system takes responsibility for the navigation.
This is where confidence, clarity and accessibility replace hesitation and delay.
Trust is the catalyst for early help-seeking
The most powerful element driving early help-seeking is trust. When we are at our most vulnerable, we instinctively prioritise safety. Logically, this means we are far more likely to engage with support avenues that we trust.
Trust is not given when it comes to workforce wellbeing services. Trust is earned through interactions that are simple, compassionate, and consistent. It is built daily, reassuring employees that the support system is for people, not problems.
So, how can we expect employees to trust workforce wellbeing systems that are disconnected, impersonal, and confusing?
Employees are keenly aware of the difference between superficial compliance and genuine care. They are looking for services that move beyond a simple “tick-box approach”. They’re seeking confidential, and personalised support that proves its value before the crisis hits.
For example, a service like Sonder builds this trust through continuous, proactive presence. By sending real-time safety notifications about local incidents or health risks, it demonstrates a genuine, protective concern for the employee’s wellbeing outside of crisis moments. Furthermore, providing confidential, self-serve wellbeing resources empowers individuals to take control of their low-level needs privately, reducing the friction and anxiety associated with asking for help.
“The fact that this app has tools in place and resources available to help navigate through difficult times is great, and then as well, talking to a real human is so comforting and helpful. I was skeptical about using the app as recommended by my workplace, but last night I found I really did need to reach out as I had no one, and I am so grateful for the support I received. What a great service; I wish every workplace had this in place.”

Member feedback survey
When employees feel safe to reach out early, the outcomes for the individual and the organisation change dramatically. Intervention happens sooner, challenges are less likely to escalate into crises, and recovery is faster. This crucial shift allows organisations to become proactive and preventative in everyday moments, instead of being reactive only when a crisis hits.
The impact of a connected model of care
Moving from a disconnected suite of services to a single entry point to holistic care offers businesses greater value and return on investment. And for employees, they have an easier way to receive the right care at the right time.
When there is one clear place to start, results are tangible:
- Employees access help sooner
- Fewer situations escalate into crisis
- Absence and unplanned leave reduce
- High-cost clinical care is used more appropriately
- Leaders gain clearer insight into emerging wellbeing risks
- Wellbeing becomes part of culture, not just a collection of services
This is the shift from a fragmented wellbeing stack to a connected system of care.
The future of employee wellbeing is simplicity

Your organisation likely does not need to add more wellbeing services. Instead, an audit and consolidated approach makes it easier for your people to access the right support at critical moments. The organisations progressing fastest are the ones simplifying, not expanding their workplace wellbeing.
When employees know exactly where to turn, everything changes. Support becomes proactive instead of reactive. Care becomes preventative rather than crisis-led. And wellbeing becomes something people use confidently, not something they remember only when they are overwhelmed.
Book time to explore what this could look like in your organisation
If you would like to discuss how a connected care model could work in your organisation, we would be happy to help. Our team can share what others are doing, what is working and how to build an easier, more human pathway to support.